This is an automatically translated article.
The article was professionally consulted with Specialist Doctor II Nguyen Quoc Viet - Interventional Cardiologist - Department of Medical Examination & Internal Medicine - Vinmec Danang International General Hospital.Arterial stenting is the optimal solution for acute cases such as acute vascular occlusion, acute myocardial infarction. However, arterial stenting also carries a risk of arterial thrombosis and embolism. Therefore, to prevent and treat embolism after stenting, antiplatelet drugs are often indicated.
1. What is an arterial stent?
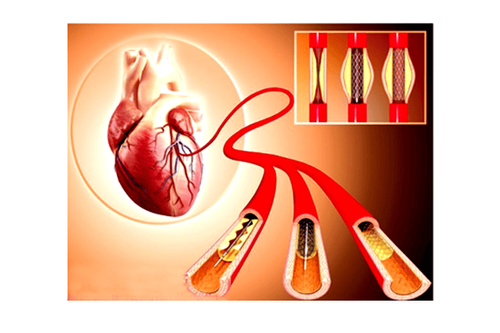
Arterial stents are metal stents used to widen blocked blood vessels, help blood flow again, reduce the risk of heart attack, and prevent brain aneurysms.Arterial stenting is a vascular intervention in specialties such as interventional cardiology, thoracic vascular,... Coronary stents are the ideal treatment option and bring a very high success rate to patients. Patients with acute myocardial infarction or chronic ischemic heart disease have significantly more than 70% coronary stenosis.
Common indications for arterial stenting are:
Acute vascular occlusion: Myocardial infarction, acute lower extremity artery occlusion,... Arterial thrombosis Carotid stenosis Thoracic aortic aneurysm, aneurysm Abdominal aortic aneurysm, cerebral aneurysm, Arterial stents such as:
Bare metal stents (BMS) are the most basic stents, with chromium-cobalt or stainless steel construction without drug coating, which carries a risk of occlusion. pulse after stent placement is highest. Drug-eluting stents (DES) are made of a metal material similar to BMS but coated with a drug that is released gradually into the lumen to prevent the growth of scar tissue that causes blockage in the artery. As a result, DES is more commonly used and the risk of arterial thrombosis is lower. Absorbable stents (BVS) are made of a self-absorbable material such as a non-metallic polymer or magnesium and are also coated with a drug to prevent the risk of post-stent embolism. After about 2 years, the BVS will dissolve in the blood and leave no trace, but still keep the artery open. Biological stents are coated with antibodies to help speed up the healing process of the arteries. Dual therapy stents (DTS) are the latest, taking advantage of stents - coated with drugs and therapeutic antibodies, reducing the risk of embolism after stenting.
2. Complications of embolism after arterial stenting
Post-stent embolism is a serious complication after vascular interventions, especially coronary interventions, with high rates of acute myocardial infarction and mortality.Diagnosis of thromboembolic complications after stenting is based on the criteria of the Association for Academic Research (ARC). Accordingly, the diagnosis of arterial thrombosis causing stent occlusion when the occurrence of acute coronary syndromes (angina pectoris, electrocardiographic changes, elevation of cardiac enzymes) is determined; evidence of thrombosis at the arterial stent site on coronary angiography (intrastent thrombus or thrombosis less than 5 mm from the proximal and distal ends of the stent); on autopsy.
Embolism after coronary stenting is classified according to the time of occurrence:
Early: Acute vascular occlusion within 24 hours or subacute within 2 to 30 days after stenting. Late: Vascular occlusion occurs between 2 and 12 months. Very late: Embolism 1 year or more after stenting. Depending on the degree of vascular occlusion, embolism after stenting causes clinical manifestations ranging from mild to severe, such as sudden continuous chest pain, ST-segment elevation myocardial infarction, and even death (10-30). %).

3. Prevention of embolism after stenting
To prevent embolism after stenting, it is important to perform an optimal coronary intervention as follows:Place the stent to cover the entire length of the lesion. Stent to the artery wall Do not dissect the coronary artery at the edge of the stent or narrow retention. Intravascular ultrasound (IVUS) plays an important role in cases where suboptimal stenting is suspected. Simultaneously, use dual antiplatelet drugs before as well as maintenance after arterial intervention. The latest recommendations from the European Heart Association and the American Heart Association both emphasize the importance of maintaining dual antiplatelet drugs after coronary stenting. To reduce the risk of post-stent embolism or death, all patients undergoing coronary intervention (e.g. balloon angioplasty or stenting) should receive aspirin in combination with a P2Y12 inhibitor antiplatelet agent. (clopidogrel, prasugrel and ticagrelor).
Duration of use of dual antiplatelet drugs after bare metal stents or drug-eluting stents is 12 months, if the risk of bleeding is not high and surgery is not required (no anticoagulants, no history of heavy bleeding). Early discontinuation of dual antiplatelet agents has been shown to be strongly associated with arterial thrombosis causing stent re-occlusion.
Longer-term dual antiplatelet therapy is recommended in the following patients:
Complex coronary intervention (left coronary trunk, persistent lesions, bifurcation lesions, interventional saphenous vein bypass). Suboptimal intervention (stent does not cover the full length of the lesion, there is residual narrowing). First-generation drug-eluting stents. Left ventricular systolic function decreased. History of post-stent embolism or thromboembolic event within the past 12 months, despite dual antiplatelet therapy. In addition, patients also need to have a healthy diet and lifestyle, including:
Eat vegetables, fresh fruits, whole grains. Reduce eating fat, salt, animal organs. Maintain a reasonable weight; avoid obesity. Control comorbidities such as diabetes, hypertension. Do not smoke, reduce alcohol and stimulants because it will harm the heart. Keep psychological stability, avoid anxiety, excessive stress. Exercise regularly, at least 150 minutes a week. In summary, post-stent embolism is a rare but serious complication of vascular interventional procedures in general and coronary intervention in particular, with a high risk of myocardial infarction and high mortality. .
To prevent this complication, it is necessary to optimize the intervention process as well as maintain long-term dual antiplatelet drugs after stenting. In the case of stent re-occlusion due to arterial thrombosis, the most effective measure is coronary reperfusion as soon as possible to reduce mortality.
Coronary stenting technique has been implemented at Vinmec International General Hospital with a success rate of up to 98%. The technique is performed by a team of highly qualified cardiologists with many years of experience in the profession. With a modern cath lab system, sterile medical equipment, and a quiet space, it helps patients recover quickly and minimize risks after stenting.
Cardiovascular Center - Vinmec International General Hospital is also applying very effectively and safely techniques of coronary angiography, balloon angioplasty, angioplasty and coronary stenting; meet the needs of timely and effective examination and treatment of acute diseases such as acute myocardial infarction, cardiogenic shock, bradyarrhythmias requiring emergency medical equipment.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.