When the balance of the microflora is disturbed, gastrointestinal fungi will take advantage of this opportunity to grow out of control and cause a series of digestive problems such as abdominal pain, diarrhea, infections of internal organs.
1. What is a gastrointestinal fungus infections?
The digestive tract plays an important role in each person's body, including a huge living microbiome, including billions of different types of bacteria, viruses, fungi, microorganisms. They are both beneficial and harmful, typically Candida Albican (both a natural fungus and a pathogenic fungus).
Fungi have only one cell and are classified as yeasts, and Candida is one of them. However, it is a special type of fungus because it has the ability to grow in a branching manner.
Complications occur when your immune system does not function optimally, giving Candida and other potentially pathogenic bacteria the opportunity to multiply beyond their normal parameters. It is this multiplication that disrupts the balance of the microbiome and can lead to signs of Candida overgrowth.
You may have heard of thrush or may have even experienced the itching and discomfort yourself. Thrush is a common manifestation of Candida overgrowth. However, the effects of Candida can be many and varied. Intestinal Candida overgrowth can lead to a variety of symptoms in your body.
Under normal circumstances, Candida does not cause any harm to your health. Your skin, genitals, mucous membranes, and intestines can all be infected with Candida without causing any significant health problems.
Candida quietly survives by using the broken down components of sugar and other nutrients to provide it with energy for reproduction, but still lives in harmony and balance with your body. Most of the time, it forms part of the normal, healthy microflora.
Candida cell walls are composed of α- and β-mannans. The Β-glucan on the fungal cell wall is recognized by your immune system. This triggers a process called phagocytosis, where immune cells called neutrophils and macrophages engulf the pathogen. It is this phagocytosis process that Candida has managed to avoid. It hides β-glucan on its surface, thereby eliminating the ability of your phagocytes to recognize and destroy invading Candida cells. Thus, Candida has adapted itself to “evade” your immune system.

2. Symptoms of gastrointestinal fungus infections
People with weakened immune systems are more likely to develop Candida overgrowth, as are the very young and the elderly.
Other factors, such as a diet high in sugar or antibiotics, have also been linked to an increase in Candida infections. Here are some typical forms of gastrointestinal yeast infections and their symptoms.
2.1. Oral thrush
Also known as oral candidiasis (candidiasis is a candida fungus infection), oral thrush is a condition in which the Candida fungus grows excessively in the mouth. Typically, white patches of thrush can be seen on the gums, roof of the mouth, tongue, tonsils, and throat.
Candida albicans usually lives in the mouth without causing any ill effects. However, in the right circumstances, it can grow out of control.
This form of candidiasis is not particularly common in healthy adults. It is more common in young and old people, and people with weakened immune systems.
In the early stages of infection, you may not notice signs of oral thrush. As it progresses, it causes a range of symptoms:
- Creamy white patches or lesions of fungus most commonly found on the tongue and inner cheeks and sometimes on the gums, tonsils and throat.
- A burning or painful sensation that may make it difficult to swallow or eat.
- Bleeding
- Cracked and red skin at the corners of the mouth
- Loss of taste
- In people with weakened immune systems, the infection can continue into the throat and can cause pain and a feeling of food constantly getting stuck in the throat.
2.2. Intestinal candidiasis
When the balance of the gut microbiota is thrown off balance by illness, antibiotic use, alcohol consumption or even stress, a poor diet high in sugar and refined carbohydrates, Candida can overgrow and cause unpleasant signs of intestinal overgrowth.
Initially, gastrointestinal candidiasis symptoms may be nonspecific. Unexplained fatigue is a common symptom. Candida often affects the way your body absorbs nutrients, so you may be deficient in magnesium, essential fatty acids, and vitamins. Other symptoms of gastrointestinal candidiasis include:
- Esophageal candidiasis: Patients often have difficulty swallowing and painful swallowing. The disease is diagnosed based on a gastrointestinal endoscopy that shows white patches in the esophagus and the presence of fungus on these white patches.
- Gastrointestinal candidiasis: Patients often have nausea, vomiting, bloating, stomach pain, or abdominal pain many times after eating.
- Intestinal candidiasis: Patients have diarrhea, food is not absorbed, leading to malnutrition, dehydration, and life-threatening. The symptoms of diarrhea when having intestinal candidiasis are no different from diarrhea caused by other causes, so it is easy to confuse. When having gastrointestinal candidiasis, patients may have symptoms such as indigestion, rapid weight loss, frequent urination, etc. The disease is diagnosed based on finding fungus in the stool through testing.
In general, the gut microbiome is necessary for digestion and the processing of certain sugars, fibers, and starches. When Candida overgrows, you may experience digestive problems, constipation, nausea, cramps, bloating, diarrhea, or gas.
Chronic and serious digestive diseases, including Crohn's disease and ulcerative colitis, are associated with Candida overgrowth in the gut.

3. Treatments of gastrointestinal fungus infection
In principle, to treat gastrointestinal fungi, it is necessary to rely on the condition of the disease (severe or mild), the patient's physical condition, and most importantly, a doctor must examine and prescribe medication.
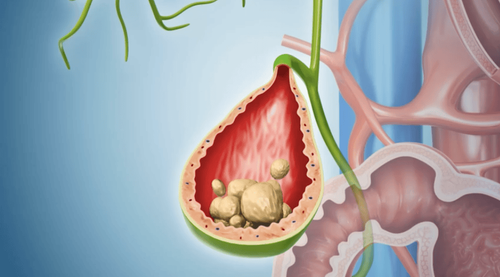
For mild and moderate Candida, ketoconazole can be used. This is a broad-spectrum antifungal drug that inhibits the alpha demethylase enzyme and prevents the synthesis of ergosterol, changes the lipids of the fungal cell membrane, and inhibits the growth of fungi. Low doses inhibit the growth of fungi, high doses kill fungi. Ketoconazole dissolves well in the acidic environment of the stomach, so it should not be used at the same time as drugs that neutralize stomach acid (such as maalox, sodium bicarbonate, etc.) or proton pump inhibitors (PPIs), because it will reduce acidity and the drug will be poorly absorbed. The unwanted effects of ketoconazole are nausea, abdominal pain, diarrhea, and more dangerously, gastrointestinal bleeding. Less common are hepatitis, cholestasis (increased bile pigment) which is more common in the elderly, women, alcoholics or those with impaired liver function due to other causes. Therefore, ketoconazole should be taken with meals for good absorption and liver enzymes (SGOT, SGPT); blood bilirubin should be checked and under the supervision of a doctor.
For severe Candida, fluconazole can be used, a broad-spectrum antifungal that is stronger than ketoconazole, belonging to the triazole group, with the effect of killing peripheral or systemic fungi. However, the drug has many unwanted effects such as toxic skin necrosis, harmful to the kidneys, especially for people with kidney disease (because the drug is mainly excreted through the urine). Therefore, it is necessary to inform the doctor when you see abnormalities (flaking, toxic skin necrosis) after automatically stopping the drug for timely treatment.
For mild digestive disorders caused by Candida albicans, nystatin (narrow-spectrum antifungal) can be used. Nystatin has the effect of inhibiting or killing fungi depending on the concentration and sensitivity of the fungus, without affecting normal bacterial flora in the body's digestive system (oral form). The most sensitive are yeasts and have a very good effect on Candida albicans. The mechanism of action of nystatin is that they bind to the ergosterol substance of the fungal cell membrane, thereby disrupting the potassium metabolism of the fungus and causing the fungus to not grow (being destroyed) but not adversely affecting the user. The unwanted effects of nystatin are that it can cause nausea, vomiting, diarrhea, digestive disorders (flatulence and bloating...) or can cause hives, rash after taking the drug, especially when using a dose of more than 5 million units per day.
Note: Patients should not arbitrarily use antifungal drugs without being examined and prescribed by a doctor.

4. The importance of diet in avoiding gastrointestinal fungus infections
For most external or internal Candida infections, the cornerstone of treatment is a low-sugar, anti-inflammatory diet. Candida loves to feed on glucose, so if your body is low on glucose, Candida doesn’t have the energy to overgrow and become detrimental to your health.
Gut dysbiosis or an imbalanced microbiome can be the cause of many conditions. Here’s a diet to help prevent gastrointestinal candidiasis:
- Avoid foods that contain sugar, such as candy, pastries, and regular soft drinks. Be careful with foods with unknown ingredients, avoid processed meats and salty foods, and avoid refined carbohydrates (including white bread and pasta) as they are quickly broken down into simple sugars as your body metabolizes them.
- Add fermented foods like sauerkraut, kimchi, live yogurt, and kefir to your diet to help balance your microbiome. Taking a probiotic supplement in pill or capsule form is a much more convenient way to ensure that your microbiome is optimal. Probiotics contain beneficial bacteria. They will help your microbiome regain balance in your body. There are many types of probiotics to choose from, but you should choose one that uses time-release technology through bioavailability.
- Increase your intake of fruits and vegetables: For example, avocados provide vitamins E and C, healthy fats, etc. Broccoli contains carotenoids that help protect you from oxidative damage that leads to wrinkles and dry skin. Walnuts contain essential fatty acids, zinc, and antioxidants.
- Olive oil and cinnamon: The search for alternative treatments for resistant strains of Candida is ongoing. Research has found that both olive oil and cinnamon oil have the ability to kill Candida isolated from blood stream infections. More than half of fluconazole-resistant Candida krusei strains were found to be susceptible to olive oil and cinnamon.
Candida forms part of the microbiome in the gut. In most people, it is likely part of a healthy microbiome and does not cause problems or disease.
Problems with Candida can arise when there is a change from the body's healthy, balanced state. This change can be due to the use of medications such as antibiotics or corticosteroids, stress, changes in hormone balance, or an underlying disease including cancer that weakens the immune system. When the balance of the microbiome is disturbed, Candida takes advantage of this opportunity to grow out of control and can cause problems ranging from fatigue and poor digestion to more serious conditions such as infections of internal organs.
Eating a diet low in sugar and carbohydrates, and taking a high-quality probiotic will help support your immune system and keep your microbiome in balance.
To arrange an appointment, please call HOTLINE or make your reservation directly HERE. You may also download the MyVinmec app to schedule appointments faster and manage your reservations more conveniently.