This is an automatically translated article.
The article is professionally consulted by Professional Advisor, Associate Professor, Dr. Hoang Dang Mich and Master, Doctor Do Xuan Chien - Department of Medical Examination and Internal Medicine - Vinmec Ha Long International General Hospital.Type 1 diabetes, also known as juvenile diabetes or insulin-dependent diabetes, is a chronic condition in which the pancreas produces little or no insulin. Insulin is a hormone needed to allow sugar (glucose) to enter cells for energy. Various factors, including genetics and some viruses, can contribute to type 1 diabetes.
1. How many types of diabetes are there?
Diabetes classification includes:
Type 1 diabetes (due to destruction of pancreatic beta cells, leading to absolute insulin deficiency). Type 2 diabetes (due to impaired pancreatic beta cell function progressing against the background of insulin resistance). Gestational diabetes (diabetes diagnosed in the second or third trimester of pregnancy and without evidence of type 1 or type 2 diabetes before). Diabetes caused by other causes, such as: neonatal diabetes or diabetes caused by the use of drugs and chemicals such as glucocorticoid use, HIV/AIDS treatment or after tissue transplantation...
2. Causes of type 1 diabetes
Type 1 diabetes is an autoimmune condition. This means that the person's immune system mistakenly attacks and destroys the beta cells in the pancreas that produce insulin, causing permanent damage.
Currently, doctors have not found the exact cause of the body's own attack on the pancreas, possibly genetic and environmental. Lifestyle factors were not associated with the cause of type 1 diabetes.
3. Mechanism of causing diabetes
Type 1 diabetes is a serious disease. The cause is damage to the beta cells of the islets of Langerhans, resulting in an absolute insulin deficiency.
Immune-mediated mechanism: The process of beta cell damage is an autoimmune process. Individuals with a genetic susceptibility are at increased risk of developing type 1 diabetes after an external attack (mumps virus, measles, coxsakie B4 and B5, retro type C). Individuals carrying HLA B8, B15 antigens, especially DR3, DR4, DR3/DR4 will have an increased risk of type 1 diabetes. The above environmental factors will attack individuals with genetic predisposition to diabetes. type 1 diabetes. Only a very small damage to the beta cells also releases antigens, stimulates the body to produce autoantibodies that trigger the autoimmune islet inflammatory response. The possible antigen is GAD (glutamic acid decarboxylase) a Kd protein located in the cytoplasm of beta cells. Autoantibodies will react with antigens.
Activated lymphocyte macrophages will gather around the islets of the pancreas causing an inflammatory response. T lymphocytes secrete chemical mediators, including interleukin-1, that have a toxic effect on beta cells. Interleukin-1 induces the formation of free radicals that damage and destroy beta cells, leading to the cessation of insulin secretion.
4. Symptoms of Type 1 Diabetes
Signs and symptoms of type 1 diabetes that can come on relatively suddenly include:
Increased thirst Frequent urination Bedwetting in children despite not having wet the bed during the night Very hungry Decreased unwanted weight Irritability and other mood swings Fatigue and muscle weakness Blurred vision
5. Risk factors for type 1 diabetes
Some known risk factors for type 1 diabetes include:
Family history. Anyone with a parent or sibling with type 1 diabetes is at risk. Genetic. The presence of certain genes indicates an increased risk of developing type 1 diabetes. Geography. The incidence of type 1 diabetes tends to increase as you move beyond the equator. Age. Although type 1 diabetes can appear at any age, it appears at two notable ages. The first occurs in children aged 4 to 7 years and the second is in children aged 10 to 14 years.
6. Complications of type 1 diabetes
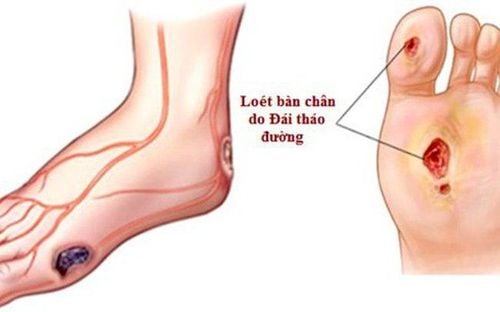
Over time, type 1 diabetes complications can affect vital organs in your body, including your heart, blood vessels, nerves, eyes, and kidneys. Maintaining normal and stable blood sugar levels can greatly reduce the risk of this complication.Heart and blood vessel disease. Diabetes greatly increases the risk of various cardiovascular problems, including coronary artery disease with angina, heart attack, stroke, atherosclerosis, and high blood pressure. Nerve damage. Excess sugar can damage the walls of the small blood vessels that feed the nerves, especially in the legs. This can cause tingling, numbness, heat, or pain that usually starts at the tips of the toes or fingers and gradually spreads upward. Nerve damage affecting the digestive tract can cause nausea, vomiting, diarrhea, or constipation. For men, erectile dysfunction is possible. Kidney damage. The kidneys contain millions of clusters of tiny blood vessels to filter waste from your blood. Diabetes can damage this delicate filtering system. This severe damage can lead to kidney failure or irreversible end-stage kidney disease, requiring dialysis or a kidney transplant. Damaged eyes. Diabetes can damage the blood vessels of the retina (diabetic retinopathy), potentially causing blindness. Diabetes also increases the risk of other serious vision problems, such as cataracts and glaucoma. Foot injury. Nerve damage in the feet or poor blood flow to the feet increases the risk of foot complications, which, if left untreated, cuts and blisters can become serious infections that eventually become fatal. may require amputation of a toe, foot, or leg.
Skin and mouth condition. Diabetes can make you more susceptible to skin and mouth infections, including bacterial and fungal infections, gum disease, and dry mouth. Pregnancy complications. High blood sugar can be dangerous for both mother and baby. The risk of miscarriage, stillbirth and birth defects increases when diabetes is not well controlled. For the mother, diabetes increases the risk of diabetic ketoacidosis, diabetic eye problems, gestational hypertension, and preeclampsia. At Vinmec International General Hospital, we always deploy a screening package for diabetes and dyslipidemia to help detect pre-diabetes early, accurately classify diabetes type, develop a nutritional regimen, according to the guidelines. Monitor to reduce the risk and complications caused by diabetes.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Article referenced source: ncbi.nlm.nih.gov