This is an automatically translated article.
The article was written by Specialist Doctor II Nguyen Trung Thanh - Anesthesiologist and Anesthesiologist, Department of Surgical Anesthesia - Vinmec Central Park International General Hospital.
Aspiration pneumonia during anesthesia is an aspiration pneumonia that occurs during anesthesia and recovery.
1. What is aspiration phenomenon?
Inhalation: is the phenomenon where substances from the pharynx or upper digestive tract enter the lungs through the larynx in subjects with loss or decrease in airway protective reflexes. The composition of the inhaled substance includes saliva, nasopharyngeal secretions, bacteria, fluids, food or contents contained in the stomach.
Clinical manifestations strongly when inhaled with a large amount or silently not noticed in the case of inhalation with a small amount. Consequences range from mild to severe with tissue hypoxia, respiratory failure, ARDS, circulatory collapse, and possibly death.
2. What is lung syndrome?
Includes inflammation caused by acid, airway obstruction and bacterial infection.
It is necessary to clearly distinguish the following two concepts:
Aspiration pneumonitis: hypoxemia, fever, tachycardia and abnormality / Chest X-ray caused by inhalation of large amounts of refluxed fluid (gastric juice, bile, .. .) Severe inflammation when pH <2.4 or volume > 2ml/kg body weight.
Aspiration pneumonia: an acute lung infection that occurs after inhaling large amounts of oropharyngeal or upper gastrointestinal secretions. Usually pH >2.5 is not enough to cause chemical pneumonitis. Bacterial strains are not usually virulent and are usually anaerobic. Preconditions associated with aspiration lung injury include risk factors along with frequent aspiration or aspiration of large amounts of oropharyngeal and gastric secretions, with or without bacteria.
It is difficult to determine whether an independent factor is associated with aspiration pneumonia or aspiration lung injury, due to the inconsistency in the usage of the terms aspiration pneumonitis and aspiration pneumonia in scientific studies.
3. Epidemiology
Inhalation in the anesthetic stick occurs at a rate of 1:2,000 - 30,000, an average of 1:2,000 - 3,000 in surgery with anesthesia, especially in emergency situations, on some special subjects such as dental hygiene poor oral health or the elderly, and tripled in thoracic surgery.
Most cases are silent or unrecognized, so the true incidence of aspiration lung damage is difficult to accurately estimate. This explains many cases of perioperative respiratory dysfunction. Most aspiration pneumonia is misdiagnosed as bacterial pneumonia and leads to inadequate treatment. The severity of lung injury after aspiration depends on the composition, volume, and acidity of the inhaled fluid as well as patient characteristics (hygiene, resistance) and varies from mild (subclinical) to respiratory failure. Respiratory.

4. Pathophysiology
Mendelson syndrome (1946): 2-stage response against acid-induced lung injury. Consists of 2 phases: phase 1 is the direct corrosive effect of low pH on airway epithelium, peaking 1-2 hours after inhalation. Phase 2 is an inflammatory response due to neutrophil activation, occurring 4-6 hours after inhalation. The mechanism involves inflammatory mediators, inflammatory cells, adhesion molecules, tumor necrosis factor α, interleukin-8, enzymes (cyclooxygenase, lipooxygenase), which play a key role. The key are neutrophils and complement. Lung infections: Stomach fluids are usually sterile under low pH conditions. However, the use of antihistamines or proton pump inhibitors can create a bacterial growth environment, cases of intestinal paralysis, intestinal obstruction or feeding through a nasogastric tube can have Gram (-) bacteria leading to lung infection if inhaled. Factors that increase the risk of lung infection are related to aspiration of a large amount of oropharyngeal or gastric juice in the above subjects and immunocompromised patients, poor oral care. Proton pump inhibitors and antihistamines do not increase the risk of aspiration but increase the risk of lung infection if aspiration is present.
5. Risk factors
Use of drugs: drugs acting on the esophageal sphincter, drugs that reduce consciousness, protective reflexes (usually used in sedation and anesthesia). Patient status: reduced consciousness, swallowing disorder or dysphagia (Parkinson's, multiple sclerosis, stroke, COPD), intestinal obstruction, emergency surgery, history of esophageal surgery, impaired coordination between swallowing and breathing, esophageal cancer, hiatal hernia, obesity. By medical staff: bad decisions, inexperience and lack of knowledge.

6. Diagnosis
Patients with risk factors for suspected inhalation when presenting with acute symptoms such as cough, dyspnea, tachypnea, shallow, cyanotic, slurred speech, hoarseness, tachycardia. Diagnosis is confirmed in the presence of oropharyngeal secretions, food, pepsin, bronchoalveolar bile, or alveolar lavage fluid.
Signs after inhalation due to acute inflammation such as fever, tachycardia, tachypnea, leukocytosis, respiratory symptoms such as cough, tissue hypoxia, chest X-ray appearance of new lesions.
Diagnose lung infection if bacteriological evidence is present.
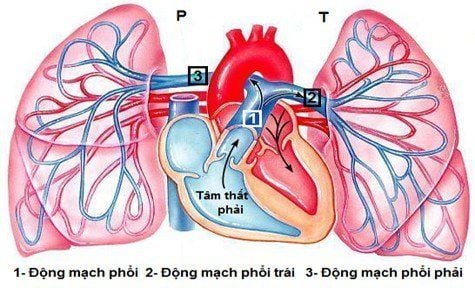
Progression of ALI/ARDS (hypoxemia, respiratory failure) increases the work of breathing, reduces lung compliance, which in turn leads to pulmonary hypertension.
Cases of aspiration without symptoms or without evidence of aspiration should be differentiated from other causes of tissue hypoxia such as acute pulmonary edema, pulmonary embolism or pneumonia. The image of pulmonary infiltrates depends on the chest X-ray (lower part of the lung, depending on the patient's position).
There is no gold standard in the differential diagnosis of aspiration pneumonia and aspiration lung injury.
Currently, Vinmec International General Hospital has been and continues to be fully equipped with modern diagnostic facilities such as: PET/CT, SPECT/CT, MRI, X-ray machine, Ultrasound, Digital imaging background removal chemistry, electrocardiogram,... blood test, myelogram,... to diagnose pulmonary embolism.
After having an accurate diagnosis of the disease and stage, the patient will be consulted to choose the most appropriate and effective treatment methods. The treatment process is always closely coordinated with many specialties to bring the highest efficiency and comfort to the patient. After undergoing the treatment phase, the patient will also be monitored and re-examined to determine whether the treatment is effective or not.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.