This is an automatically translated article.
Posted by Specialist Doctor II Pham Thi Khuong - Infectious Doctor - Pediatric Center - Vinmec Times City International Hospital
Anthrax is an acute infectious disease caused by the bacterium Bacillus Anthracis. The disease can be transmitted to humans through contact with sick animals or diseased animal products.
Anthrax was among the first discovered Woolsorters' disease. The first description of anthrax is known from 1491 BC, causing disease in both animals and humans. By the 17th century, epidemics had killed many people and animals throughout Europe. In 1881, Pasteur worked on making a vaccine and in 1939 Sterne successfully made an anthrax vaccine.
Animals commonly infected are buffaloes, cows, goats, sheep, herbivores. The disease can be transmitted to humans through contact with sick animals or diseased animal products.
1. What is the cause of anthrax?
Copied from the Centers for Disease Control and Prevention. The Public Health Image Library (PHIL). Available at: https://phil.cdc.gov/Details.aspx?pid=2105
Bacillus anthracis is the causative agent of anthrax and is transmitted through 4 routes of infection: Respiratory, gastrointestinal, percutaneous and injecting. Gastrointestinal anthrax is rare, but can rapidly lead to systemic illness, severe and fatal in 25%-60% of cases. The pathogenic mechanism of gastrointestinal anthrax remains unclear.
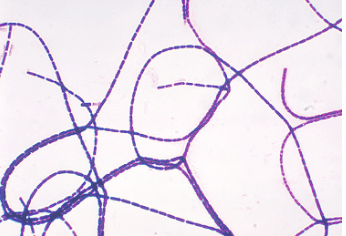
Mẫu cấy nhuộm Gram này cho thấy các chuỗi vi khuẩn Bacillus anthracis hình que, gram dương.
2. Epidemiological characteristics
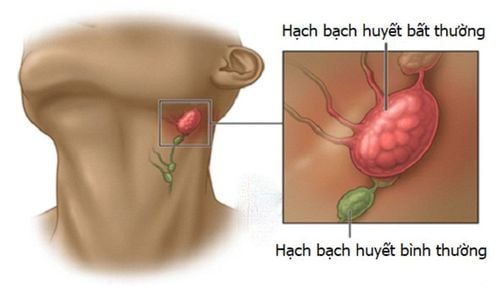
Anthrax is distributed over time, place, and people: The disease is endemic in South America, Central America, Southern and Eastern Europe, Asia and Africa. The disease usually occurs in people who are involved in the breeding and slaughter of herbivores, in leather and fur processing workers; veterinary staff...3. Source of anthrax transmission
Animals are usually herbivores including wild animals as well as livestock that spread the bacillus in bleeding, at death. In the external environment, spore-forming bacilli and B. anthracis spores are very resistant to harsh environmental conditions and sterilization, the bacteria can survive in the soil for many years after the infected animal has been infected. be destroy.
Animal skin contaminated with bacilli, even though it has been processed, can harbor spores for many years and is a worldwide vector of disease. The incubation period ranges from a few hours to 7 days, with most cases occurring within 48 hours of exposure. Human-to-human transmission is very rare. Infested objects and soil can last for decades.
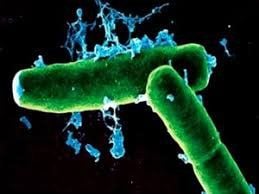
Vi khuẩn có thể truyền bệnh than từ động vật sang người
4. Mode of transmission
B. anthracis can enter the body in 4 ways: oral, transdermal, inhaled and direct injection through the gastrointestinal tract. Specifically:
4.1. Gastrointestinal
Common anthrax usually affects the gastrointestinal tract. The term "gastrointestinal anthrax" is used to refer to cases of organisms entering the gastrointestinal tract. Most anthrax in nature occurs in herbivores and is acquired through the gastrointestinal tract. Spores contaminate when the grass is ingested. The organism then invades the intestinal-associated lymphoid tissue, particularly at Peyer's plaques. An in vitro study using a cell line derived from human M cells showed that, as in a number of other infections, M cells play a role in bacterial cell uptake. . In humans, gastrointestinal anthrax occurs after ingestion of contaminated and undercooked meat. Once ingested, anthrax bacilli are transported to the mesenteric lymph nodes. Later, hemorrhagic mesenteritis, ascites, and sepsis may occur. One case was described in a patient playing a drum with contaminated animal skin. One investigation suggested that the patient was exposed to B. anthracis spores at the drumming event, resulting in gastrointestinal anthrax rather than inhalation anthrax. There is no evidence of transmission of anthrax from contaminated animal milk. The disease is transmitted in herbivores through contaminated feed and soil. Between omnivores and carnivores, the disease is transmitted through contaminated food and food products. Wild animals spread disease by ingesting carcasses of animals that have died from anthrax. Birds that feed on dead animals can also spread disease from one area to another.
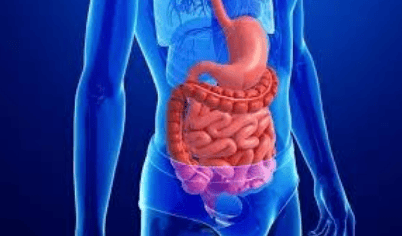
Bệnh than lây bệnh qua đường tiêu hóa
4.2. Transmitted through the skin
Percutaneous invasion can occur by two mechanisms. Although abrasions are thought to be necessary to cause skin infections, the organism is also capable of penetrating hair follicles. Once B. anthracis spores are introduced subcutaneously as vegetative organisms and begin to multiply, the production of an anti-phagocytic cyst facilitates local spread, and exogenous reproduction The toxin causes marked edema and tissue necrosis. A blister with extensive surrounding edema is a sign of cutaneous anthrax. The disease is transmitted by contaminated soil from infected animals or by the use of fertilizers made from infected animal bones used to fertilize gardens and fields.
4.3. Disease transmission through needles
Recently, another type of anthrax infection has been identified among people who inject heroin in Northern Europe. This type of infection has never been reported in the United States. Symptoms may be similar to those of cutaneous anthrax, but there may be an infection deep under the skin or in the muscle where the drug was injected. Needle-borne anthrax can spread throughout the body faster, making it harder to recognize and treat. Many other more common bacteria can cause infections in the skin and at the injection site.

Lây truyền qua kim tiêm là một phương thức lây truyền
4.4. Spread through the respiratory tract
The classical understanding of inhalation anthrax is that the spores must reach the bronchioles and alveoli, where they spread to the mediastinal lymph nodes by a process that appears to involve the bronchioles. dendritic cells. There, they germinate and cause hemorrhagic mediastinitis before dissemination. More rarely, inhaled spores can cause disease of the nose, pharynx, or larynx, or the patient can develop primary meningitis, where the most likely route of entry is the respiratory tract. Airborne anthrax spores > 5 microns in size are not dangerous to the lungs, because they are trapped in the nasopharynx or are eliminated by the mucosal transport system. Spores ranging in size from 1 to 5 microns are deposited in alveolar or alveolar ducts. These spores are phagocytosed by alveolar macrophages and transported to the mediastinal lymph nodes, where they multiply and cause hemorrhagic mediastinitis. Sepsis is a nearly common complication of untreated mediastinal infection. Larger particles can lodge in the upper respiratory tract and cause an infection, which can spread from that location.
Random infections can occur in laboratory workers. However, regardless of the infection, local infection can occur. If not treated early, it can lead to sepsis.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Clinical manifestations and diagnosis of anthrax; Daniel J Sexton, MD This topic last updated: Jan 24, 2019. Tonry JH, Popov SG, Narayanan A, Kashanchi F, Hakami RM, Carpenter C, Bailey C, Chung MC . In vivo murine and in vitro M-like cell models of gastrointestinal anthrax. Microbes Infect. 2013 Jan;15(1):37-44. Epub 2012 Oct 26. Treatment of anthrax; Kenneth H Wilson, MD. This topic last updated: Jan 24, 2019 January 14, 2016,Content source: Centers for Disease Control and Prevention, National Center for Emerging and Zoonotic Infectious Diseases (NCEZID)