This is an automatically translated article.
Posted by Doctor CKII Nguyen Thi Hoai Nam - Department of Surgical Anesthesia - Vinmec Central Park International General HospitalIn the last few years, there have been occasional reports of anesthetic poisoning cases in which patients could be treated promptly or sometimes more seriously, causing death. So what is anesthetic poisoning and what should be understood about this complication?
1. Anesthesia and anesthetic methods
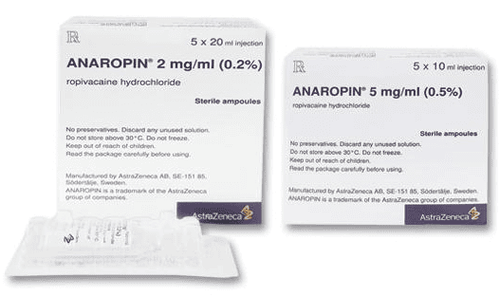
Local anesthetics are drugs that have the property of blocking nerve conduction when in contact with nerve tissue at appropriate concentrations. After a period of time, nerve function is completely restored, there is no damage or sequelae in nerve cells and fibers. Anesthesia does not cause loss of consciousness, only reduces or loses sensation and movement. There are many types of anesthetics that are packaged in different strengths and concentrations depending on the method of anesthesia.
Anesthesia is a method of temporarily reducing or losing sensation in a part or area of the body, but without losing consciousness, the patient is still awake. Commonly used anesthetic methods: Skin and mucosal anesthesia, local anesthesia, infiltration anesthesia, plexus anesthesia, spinal anesthesia, epidural ...
2. Local anesthetic poisoning
To be more precise, in medical terms it is systemic anesthetic poisoning (L ocal A naesthetic S ystemic T oxicity (LAST ). This is a serious and potentially fatal adverse reaction when plasma concentrations of the drug exceed the therapeutic threshold.
Anesthesia poisoning occurs when:
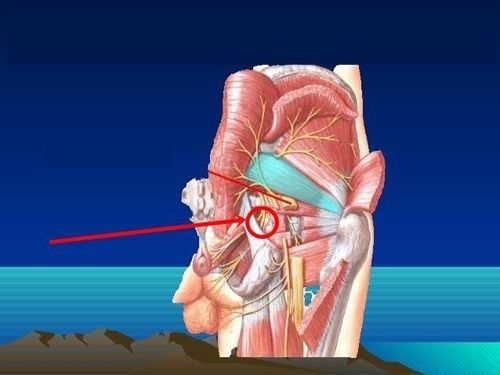
When the drug is unintentionally injected into a blood vessel (usually occurs)

Ngộ độc thuốc tê xảy ra khi thuốc tê được tiêm vào mạch máu
Absorption from the tissue at the injection site in local anesthesia When repeated injections do not balance the elimination of the drug This causes the drug in the blood to be higher than the maximum allowable concentration, leading to a toxic dose means drug poisoning.
3. What are the signs and symptoms of anesthetic poisoning?
Signs of anesthetic toxicity usually appear from 1-5 minutes but can be later within 60 minutes after injection, even after 1-12 hours. Local anesthetic toxicity manifests in the central nervous system 36%, the cardiovascular system 28% and both nervous and cardiovascular systems accounted for 36%.
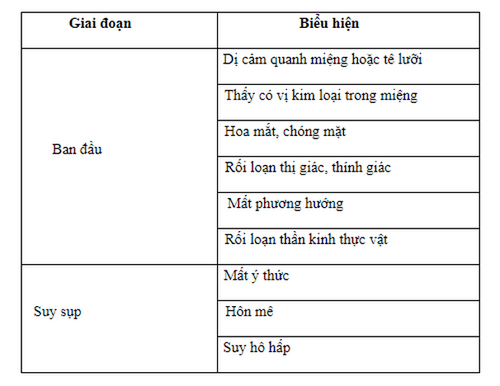
Central nervous system manifestations: Usually precedes cardiovascular signs, including 2 phases of initial excitability and collapse
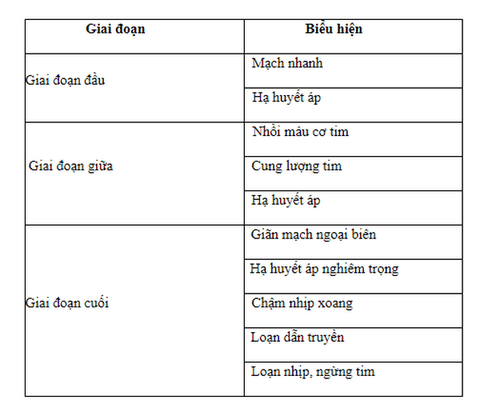
Manifestations on the cardiovascular system: Depending on the degree of poisoning, there can be 3 stages
4. When to think of anesthetic poisoning?
Blood tests can help measure the concentration of anesthetic in the blood. However, the results may not correspond to the clinical presentation. In addition, it often takes time to do tests while the progression of anesthetic poisoning is often fast and requires the hospital to handle it as quickly as possible to avoid severe neurological and cardiovascular effects. Therefore, the diagnosis is often based on clinical symptoms, especially neurological signs in the initial arousal phase. Note that it is important to distinguish poisoning from anesthetic allergy because it can affect the emergency process. Allergic reactions to local anesthetics are rare.
5. What to do when suspecting that the patient has anesthetic poisoning?
Stop injecting local anesthetics immediately Call for medical help Consider using Lipid emulsion at the onset of toxicity according to the American Society of Regional Anesthesiology and Anesthesia (ARSA) protocol and of the Ministry of Health Use an anesthetic poisoning first aid kit Notify the CPR because resuscitation may take a long time Airway control: Ventilate with 100% oxygen and use a raised airway high if needed. Anticonvulsants: Benzodizepin is preferred, Propofol should be avoided. Treat hypotension and bradycardia if present. at least 2 hours if only CNS manifestations.

Người bệnh cần được thông khi với Oxy 100% giúp kiểm soát đường thở
6. Factors that increase the risk of anesthetic toxicity
Type of anesthetic: Bupivacaine toxicity > Lidocaine > Ropivacaine > Mixed anesthetic > Levobupivacaine
The higher the concentration of local anesthetic, the larger the volume, the risk of toxicity
Location, type of anesthetic:
Area of large vessels increase the risk of injecting drugs into the blood vessel (intermediate trapezius) Increase the risk of absorption of local anesthetics (numbness of the scalp, pleura, bronchial mucosa) Intercostal anesthesia > sacral anesthesia > epidural anesthesia > arm plexus anesthesia > subcutaneous anesthesia 1 dose injection > continuous infusion Patient
Cardiovascular, renal, liver dysfunction Elderly Children Children Pregnant women

Phụ nữ có thai thuộc nhóm đối tượng có yếu tố nguy cơ ngộ độc thuốc tê
To reduce the risk of anesthetic toxicity, it is necessary to:
Use the smallest effective anesthetic dose Identify the patient's risk factors Regional anesthesia under ultrasound guidance Use a test dose Repeated reverse suction of the syringe during injection of anesthetic to avoid injecting into blood vessels Discuss with the surgeon the dose of anesthetic used during surgery to avoid overdose. Monitor patient continuously with standard Monitor Communicate and talk to patient continuously during anesthesia to detect early signs of neurotoxicity. At Vinmec Health System, patients are always evaluated before surgery according to the pre-anesthesia examination process to have an appropriate anesthetic and anesthetic plan. The modern monitor system fully monitors vital signs during and after surgery to help detect the patient's abnormalities early in order to promptly handle possible complications. Developing regional anesthesia under ultrasound guidance is Vinmec's strength, helping patients to reduce pain well and safely during and after surgery.
To register for examination and treatment at Vinmec International General Hospital, you can contact Vinmec Health System nationwide, or register online HERE.
SEE MORE
Is cesarean delivery painful? Spinal anesthesia for caesarean section Differentiate between epidural and spinal