This is an automatically translated article.
The article was professionally consulted by Specialist Doctor I Nguyen Duc Thong - Anesthesiologist - General Surgery Department - Vinmec Danang International Hospital. The doctor has 14 years of experience in the field of Anesthesia.Laparoscopic surgery for facial paralysis is a difficult surgery with a long time to perform. Endotracheal anesthesia is an anesthetic method used to perform laparoscopic surgery for facial paralysis.
1. Endoscopic neurosurgery to treat facial paralysis
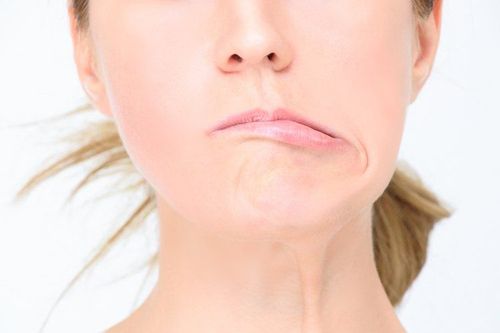
Nerve VII is responsible for controlling movement of facial muscles. Therefore, when the VII nerve is damaged, whether the damage is central or peripheral, it will also cause paralysis of the facial muscles. Patients with facial paralysis will have clinical symptoms such as:Facial skin on the side of paralysis is delayed, muscle tone loss, blurred nasolabial folds; Lower lip sag, difficult to close the mouth, eating and drinking; Delayed lower eyelids, closed eyelids, or watery eyes, possibly dry or ulcerated corneas. There are many causes of nerve damage to the VII nerve causing facial paralysis such as: trauma to the skull base to cut, crush or compress the nerve; as a result of surgery to remove neuroma VII, surgery on the temporomandibular joint; due to parotid-submandibular infection; Cerebrovascular accident, brain tumor,...
Endoscopic surgery for facial paralysis is one of the treatments for VII nerve palsy, helping to restore facial balance and overcome disorders caused by facial paralysis. nerve paralysis, muscle paralysis caused. The anesthetic method used for endoscopic neurosurgery to treat facial paralysis is endotracheal anesthesia.
2. Anesthesia in endoscopic neurosurgery for facial paralysis

2.2. Preparation To perform endotracheal anesthesia in endoscopic neurosurgery for facial paralysis, a specialist nurse and anesthesiologist are required.
Regarding the means, it is necessary to have:
Anesthesia machine system with breathing, equipment to monitor vital functions (pulse, electrocardiogram, blood pressure, oxygen saturation, breathing rate, temperature), monitor anesthesia Entropy , monitor muscle tenderness (TOF), oxygen source and other machines such as defibrillators, sputum aspirators, heaters, infusion machines... Laryngoscopes, endotracheal tubes of all sizes, straws, mask, squeeze ball, oropharyngeal cannula, Magill pliers, soft mandrin; Lidocaine 10% spray, Salbutamol spray; Means should be prepared to prevent difficult intubation: Cook tube, laryngeal mask, flexible bronchoscope, tracheostomy kit, mouth opener,... To prepare for induction For endotracheal anesthesia, the doctor will examine the patient under anesthesia before surgery to detect and prevent risks, explain to the patient the purpose and procedure for the patient to cooperate. Assessment of intubation is difficult in the patient to perform if conventional intubation procedures are not feasible. The doctor can prescribe the patient to use sedation from the night before surgery if necessary.
2.3. Techniques for performing anesthesia in endoscopic neurosurgery for facial paralysis

Perform anesthetic induction with drugs:
Sleeping pills: choose one of the drugs such as intravenous anesthetics (propofol, etomidat), volatile anesthetics (sevoflurane, desflurane,...) Pain relievers: fentanyl, sufentanil ... Muscle relaxants: rocuronium, vecuronium, succinylcholine... An endotracheal tube will be placed when the conditions are met that the patient is in deep sleep and has enough muscle relaxation (in most cases). There are two techniques that can be used for intubation under general anesthesia: oral intubation and nasal intubation.
Oral intubation technique
The doctor (or anesthesiology specialist nurse) opens the patient's mouth, inserts the laryngoscope to the right of the mouth, moves the tongue to the left, pushes the light deep, coordinates With the right hand, press down on the cricoid cartilage to find the epiglottis and glottis. Perform rapid induction of anesthesia and Sellick maneuver in case of full stomach (press the cricoid cartilage 20-30 kg as soon as the patient loses consciousness until the intubation is complete). Pass the endotracheal tube gently through the glottis, stopping when the balloon of the endotracheal tube passes 2-3 cm through the vocal cords. Gently withdraw the laryngoscope, then inflate the endotracheal balloon. The doctor will listen to both lungs and see the EtCO2 chart results to check that the endotracheal tube is in the correct position or not. If it is in place, the doctor will secure the tube with tape and place the cannula in your mouth to avoid biting the tube if necessary. Nasal intubation technique
The doctor chooses the side of the nose that will intubate the airway, instills vasoconstrictor drugs such as naphazoline, otrivine, etc. The endotracheal tube was lubricated with lidocaine ointment through the nostrils. Open the patient's mouth, insert the laryngoscope to the right of the mouth, slide the patient's tongue to the left, push the lamp deep, and coordinate with the right hand to press the cricoid cartilage to find the epiglottis and glottis. In favorable cases, proceed to gently insert the endotracheal tube through the glottis, stopping when the balloon of the endotracheal tube passes 2-3cm through the vocal cords. Using Magill pliers to guide the tip of the endotracheal tube into the correct glottis, the assistant pushes the endotracheal tube from the outside in difficult cases. Remove the laryngoscope gently, inflate the endotracheal balloon. The doctor checks that the endotracheal tube is in the correct position by listening to the lungs and checking the EtCO2 results. The endotracheal tube is secured with adhesive tape. In case of unsuccessful implementation of the above two procedures, the doctor will switch to performing the difficult endotracheal intubation procedure using a flexible bronchoscope for intubation.
During surgery, to maintain general anesthesia, the patient will be used intravenous or volatile anesthetics, analgesics, muscle relaxants. The depth of general anesthesia will be closely monitored based on parameters such as heart rate, blood pressure, sweating, tearing (PRST); MAC, BIS, Entropy. The patient's breathing is controlled by a ventilator. Vital signs and endotracheal tube status are always closely monitored. Evaluation of muscle tenderness is based on the extensometer TOF.
After endoscopic surgery for facial paralysis is over, the endotracheal tube is removed when the patient meets the following criteria:
Patient is awake, can follow orders, raises his head for more than 5 seconds, TOF > 90% , Entropy 90 -100, body temperature > 35°C. Self-breathing, respiratory rate within normal limits, stable blood pressure; No complications of anesthesia and surgery.
3. Possible complications during anesthesia in endoscopic neurosurgery to treat facial paralysis and how to handle it
3.2. Hemodynamic disorders During general anesthesia for endoscopic neurosurgery to treat facial paralysis, patients may experience hypertension, hypotension, bradycardia, tachycardia, and arrhythmias. .. The doctor will treat according to the specific symptoms and causes of each specific hemodynamic disorder.
3.3. Incident due to intubation Failure to intubate: The anesthesiology team will switch to a difficult intubation procedure or switch to another anesthesia method. Misplaced in the stomach: The anesthesiologist team will re-intubate the endotracheal tube. Vocal-tracheal-bronchospasm: If ventilation is difficult or impossible, with crackles or muted lung auscultation, the patient will be provided with adequate oxygen, added sleeping pills and muscle relaxants, ensuring ventilation and giving bronchodilators, corticosteroids. If breathing is still not controlled, the anesthesia team will apply a difficult intubation procedure. Trauma during intubation: Injuries that can occur during intubation such as bleeding, tooth fracture, vocal cord damage, foreign object fall into the airway,... Handling depending on the specific injury. 3.4. Respiratory complications If the endotracheal tube is folded, retracted, pushed deep into one lung, dropped or opened the respiratory system, the oxygen source is exhausted, the soda is ineffective, ... will lead to hypoxia and lament. The anesthesiologist team will immediately ensure ventilation, provide 100% oxygen and address the cause.
3.5. Complications after extubation After extubation, patients may experience complications such as respiratory failure, sore throat, hoarseness, laryngotracheal-bronchospasm, upper airway inflammation, and narrowing. larynx-trachea,... The treatment will be according to specific symptoms and causes.
Vinmec International General Hospital is one of the hospitals that not only ensures professional quality with a team of leading medical doctors, modern equipment and technology, but also stands out for its examination and consultation services. comprehensive and professional medical consultation and treatment; civilized, polite, safe and sterile medical examination and treatment space.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.