This is an automatically translated article.
The article is professionally consulted by Master, Doctor Ta Quang Hung - Department of General Surgery - Vinmec International General Hospital Da Nang. The doctor has more than 10 years of experience in teaching and practicing in the field of Anesthesia.Neuroradiological intervention is an increasingly widely used technique in the diagnosis and treatment of central nervous system diseases. Anesthesia plays an important role in facilitating smooth neuroradiology procedures, giving the patient the best chance of treatment.
1. What is neuroradiological interventional technique?
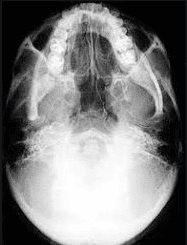
Intravascular X-ray techniques in the diagnosis and treatment of central nervous system diseases are called interventional neuroradiology or endovascular neurosurgery. This is a combination of traditional neurosurgery methods and neuroradiology.More broadly, neuroradiological intervention is a method of using drugs and instruments for intravascular treatment. This is a minimally invasive neurosurgery method, which is increasingly widely used today. If in the past, with diseases that could not be treated or could only be treated with open surgery, now treatment with interventional radiology can be considered.
2. Anesthesia method for neuroradiological intervention patients
Anesthesia is an anesthetic method that causes the patient to lose sensation, pain, and muscle relaxation during the procedure. This is one of the particularly important stages, deciding the success of the surgery.More and more pathologies are treated with neuroradiological intervention, creating many challenges for the anesthesiologist.
2.1 Notes in Interventional Anesthesia Neuroradiology Keep the patient immobile during the procedure to facilitate radiography; For patients to wake up quickly to serve the assessment, neurological monitoring; Anticoagulation treatment; Control complications during neuroradiological intervention such as bleeding or embolism; Guidelines for the internal management of critically ill patients during transfer in and out of the radiology room; Radiation safety issues. 2.2 Patient preparation Detailed assessment of overall health, pathology, effects on organs, imaging and background neuropathy,...; Assess baseline blood pressure and cardiovascular reserve as often during the intervention it will be necessary to correct blood pressure and predict treatment-related disorders; Determine history of renal failure and use of metformin, check renal function before administering contrast media. Do not use metformin in diabetic patients with renal failure. If eGFR <60 ml/min, discontinue metformin after contrast medium; A negative or non-pregnant pregnancy test is needed in women of childbearing age because the procedure uses high doses of radiation - which can adversely affect the fetus; The patient should have blood tests before the procedure, including methods of total blood cell analysis, blood group testing, coagulation, urea and electrolytes, saving blood samples in case of bleeding; Determine history of allergy to iodine and shellfish such as shrimp, crab, shellfish, snail,... Note to patients with previous allergy to protamine and contrast medium; patients with arthritis in the neck and back; Patients at risk of respiratory failure when using sedatives,...

The choice of anesthetic is mainly based on cardiovascular and cerebrovascular problems. Patients can be anesthetized with inhalational, intravenous, or a combination of the two, ensuring minimal hemodynamic changes, rapid control of the depth of anesthesia, and rapid, smooth awakening.
Use of intravenous sedation The main benefit of intravenous sedation is that it allows continuous assessment of neurological function throughout the procedure, avoiding hemodynamic changes due to intubation and anesthesia. The disadvantage of this is that it does not protect the airway against the risk of aspiration, which can cause hypoxemia and hypercapnia. In addition, the use of intravenous sedation can also cause sudden movements of the patient, causing delay in the treatment of neurological emergencies.

The sedatives used are propofol and dexmedetomidine.
Then, the doctor will give the patient anticoagulation to minimize the complications related to thromboembolism, and prevent thromboembolism during and after the neuroradiological intervention procedure. . During the procedure, there may be some complications such as bleeding, embolism, extraneural complications, hematoma, etc.
When performing neuroradiological intervention, it is necessary to carefully evaluate the risk of anesthesia from distance and radiation exposure, select an appropriate anesthesia method. At the same time, it is necessary to closely follow up in the time after the procedure to identify problems early for timely intervention.
Vinmec International General Hospital with a system of modern facilities, medical equipment and a team of experts and doctors with many years of experience in medical examination and treatment, patients can rest assured to visit. examination and treatment at the Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.














