This is an automatically translated article.
The article was professionally consulted by Specialist Doctor II Nguyen Binh - Department of General Surgery - Vinmec Ha Long International Hospital. Doctor Nguyen Binh has more than 20 years of experience in the field of anesthesia and resuscitation.The most commonly used procedure in the treatment of solitary large liver cysts is the excision of the liver cyst. Surgery can be performed laparoscopically or open surgery, but the most common option currently is laparoscopic. In which, endoscopic liver cystectomy is a complicated technique and requires the operator to be proficient.
1. What is a liver cyst?
Simple hepatic cysts are common and benign lesions. Very few patients with liver cysts present with symptoms and require medical intervention. These epithelial cells secrete follicular fluid, whose composition is similar to that of plasma. Like white blood cells, cyst fluid does not contain bilirubin or amylase. Rarely, there is communication between the cyst and the bile and there is a yellow color of bile in the cyst fluid.2. Laparoscopic hepatectomy
2.1. Indications and contraindications Laparoscopic surgery to remove liver cysts from the body is called laparoscopic liver cystectomy.Indications: Only laparoscopic liver cystectomy is performed when the following factors are satisfied:
Presence of solitary liver cyst or large liver cyst at risk of rupture Thin cyst wall Cyst is located in the middle segment, Anterior and lateral Contraindications: Do not perform laparoscopic liver cystectomy if
Germs appear in the cyst (superinfected cyst) - there is an anastomosis between the cyst and the biliary tree. Suspected malignant cyst, liver fluke cyst Location of liver cyst in posterior segment 2.2. Procedure for performing laparoscopic liver cystectomy Things to keep in mind when performing this technique:
The patient needs to be enema to clean the colon. On the morning of surgery, the patient needs to fast and disinfect the abdomen. Use prophylactic antibiotics at the time of skin incision. Patients need to breathe oxygen, closely monitor pulse, blood pressure, temperature, urine, drainage within the first 24 hours. On the first day after surgery, the patient should have a complete blood count test, basic coagulation, biochemical liver and kidney function, and electrolytes. The patient can eat again, food from liquid to solid gradually, the amount gradually increases on the 3rd day after surgery. 2.3. Benefits of laparoscopic liver cystectomy laparoscopic liver cystectomy is the preferred surgical method today because it has many advantages, such as:
Less invasive to the patient's body Patient's health is guaranteed and safe About 8 hours after surgery, the patient can recover, eat and travel. Short hospital stay Saves on treatment costs compared to other methods. However, like other surgical techniques, laparoscopic liver cystectomy may also have undesirable effects.

3. Endotracheal anesthesia for laparoscopic liver cystectomy
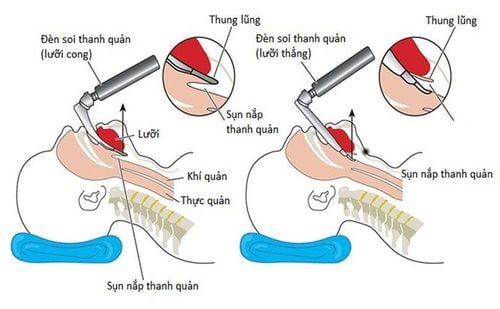
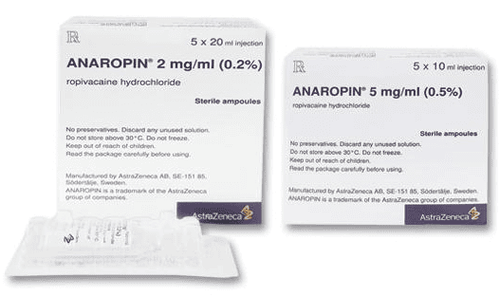
Endotracheal anesthesia is a technique of general anesthesia through endotracheal tubes for the purpose of controlling breathing during surgery and resuscitation after surgery for patients. This method requires medical facilities to have all the necessary modern equipment, and the operator must be trained and proficient in techniques.3.1. Steps to carry out endotracheal anesthesia for laparoscopic liver cystectomy Check records Check the patient Technical implementation: The general steps are: Patient position: supine, 100% oxygen at a rate of 3-6 l/min at least 5 minutes before induction of anesthesia. Install the tracker. Set up transmission. If necessary, pre-anesthesia can be performed. Induction of anesthesia: sleeping pills Pain relievers Muscle relaxants (if necessary) The condition for intubation is that the patient must sleep deeply and have enough muscle relaxation. Carrying out oral intubation: insert the endotracheal tube through the mouth, put the cannula in the mouth to prevent the patient from biting the tube (if necessary). Maintain anesthesia with intravenous or volatile anesthetics, analgesics, and muscle relaxants (if needed). Control the patient's breathing with a machine. Criteria for extubation: The patient is awake, following the doctor's orders. Patient can raise head for more than 5 seconds, TOF >0.9. The patient is breathing on his own, the respiratory rate is within normal limits. Pulse and blood pressure are stable. Temperature > 35 degrees C. The patient had no complications of anesthesia and surgery. 3.2. Complications and management in endotracheal anaesthesia laparoscopic liver cystectomy. Reflux of gastric juice into the airway Gastrointestinal fluid was found in the oral cavity and airways. At that time, it is necessary to immediately aspirate the fluid, place the patient in a low position, and tilt the head to one side. Place the endotracheal tube quickly and clear the airways immediately. Then it is necessary to monitor for lung infections. Hemodynamic disorders Patients with hypotension or hypertension, cardiac arrhythmias (tachycardia, bradycardia or arrhythmia). Treatment depends on the specific symptoms and cause.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.