This is an automatically translated article.
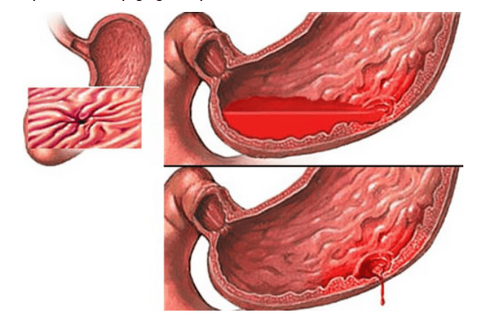
Posted by Master, Doctor Mai Vien Phuong - Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International HospitalUpper gastrointestinal bleeding was defined as bleeding originating from the esophagus to the ligament of Treitz of the duodenum and was classified as gastrointestinal bleeding not due to ruptured varices and bleeding due to ruptured varices. What are the advantages and disadvantages of new endoscopic treatment modalities for gastrointestinal bleeding not due to varicose veins?
1. Two groups of causes of upper gastrointestinal bleeding
The cause of upper gastrointestinal bleeding due to varices rupture (UGIB) is usually in patients with cirrhosis, as a result of portal hypertension, causing varicose veins of the stomach and esophagus, in the center of aneurysms, antrum of the antrum. or duodenum. The endoscopic treatment of choice for bleeding from esophageal varices is venous ligation. Bleeding from gastric varices is treated with an injection of cyanoacrylate. Vasopressor therapy as well as antibiotic therapy is initiated before or at the same time as endoscopy.
Upper gastrointestinal bleeding from varicose veins remains a common clinical problem globally. It is associated with high mortality, morbidity and costs of the health care system. Despite the continued improvement of therapeutic endoscopy, the 30-day rate of recurrent bleeding and associated mortality is an ongoing problem.
The Food and Drug Administration currently has approved conventional or conventional therapeutic endoscopic modalities including epinephrine injection, argon coagulation, heating probes, and OTSC bronchoscope clamps, with may be used alone or in combination to reduce the risk of bleeding. Recently, new advanced endoscopic devices have received more attention for initial treatment of bleeding lesions and as an adjunct when conventional therapies fail to achieve hemostasis. This review highlights emerging endoscopic modalities used in the management of upper gastrointestinal bleeding from ruptured varicose veins such as over-the-scope clip (OTSC), Coagrasper, hemostatic spray, excision Radiofrequency ablation, cryotherapy, endoscopic flexible gastrointestinal suture devices and endoscopic ultrasound therapy for arterial occlusion. In this review, technical aspects of common procedures, outcomes in terms of safety and efficacy, and advantages and limitations in the management of non-ruptured upper gastrointestinal bleeding will be discussed. vein.
2. Advantages and limitations of hemostatic methods in the treatment of upper gastrointestinal bleeding due to varicose veins
2.1 Advantages of hemostasis in upper gastrointestinal bleeding Emerging endoscopic treatment OTSC Clip Clamp Simple to use Effective for ulcers larger than 2 cm in diameter, or vascular > 2 mm More technically feasible and effective for larger, deep and fibrous ulcers 2.2 Disadvantages of hemostasis in the treatment of upper gastrointestinal bleeding Difficulty closing sclerotic, chronic lesions Complicated and too extensive with OTSC Special endoscopic skills are not needed Time-consuming, especially in emergency situations (after identifying the source of bleeding, the scope must be removed to attach the OTSC system on endoscope and reinsertion to implement the endoscopic gastrointestinal suture, endoscopic elastic ligation (EVL) clip, which involves a reduction in treatment portions, bleeding control, and the need for blood transfusion. EVL hyperplastic gastric polyp was safe, technically simple and highly effective in this patient with complete removal of GAVE. safest and most effective due to the large surface area of the clamp and the non-slip jaw design providing a mechanical compression effect to the surrounding tissuesCoagulation may not be complete due to electrical leakage if injury submersion in water or extensive tissue or surface area injury. The risk of perforation is extremely low, as coagrasper operates at a lower voltage than other heat treatments that coagulate tissues without any carbonization and without extending to deeper tissue. Because of the devices used for soft coagulation, including disposable hemostatic forceps, this approach may be appropriate only for centers that perform routine ESD submucosal dissections. Clamps that can be used to treat multiple bleeding sites have proven to be cost-effective.
Several cases of aspiration pneumonia have been reported as radiofrequency electrocautery, feasible and safe in ablation of GAVE vascular metaplasia lesions. Endoscopic skill is required to perform RFA, which is capable of providing high energy coagulation of superficial mucosa including blood vessels.
Precise positioning of the gastric mucosa with the electrode is required to allow efficient delivery of electrical energy, which means that the endoscope may have to be removed, rotated, and reinserted several times. . Newer rotatable internal combustion catheters can avoid this drawback but have a smaller surface area. Wider surface area covers mucosa due to different electrode sizes. Area contact technique distributes and penetrates energy evenly so that deeper submucosal vascular channels are coagulated
3. Endoscopic ultrasound guided therapy for arterial occlusion
EUS-guided bleeding therapy has been shown to be feasible and safe for peptic ulcer disease, Dieulafoy's lesion, hemorrhagic tumour, etc., due to its direct visualization and targeting capabilities. into the bleeding vessel with a specific therapy and then confirm hemostasis with real-time Doppler ultrasound, which is a significant advantage of EUS-guided therapy.
Endoscopic skills are required to perform endoscopic ultrasound. EUS-guided arterial occlusion therapy is more resource intensive than other conventional endoscopic hemostasis procedures. The topical therapies i.e. Hemospray and Endoclot are easy to use, safe and effective, and cost-effective. May be used for gastrointestinal bleeding due to malignancy
Theoretically possible side effects of Hemospray include embolism, intestinal obstruction and allergic reaction to the powder. If hemostasis is not successful, there is the disadvantage that the powder adheres to the mucous membrane which may limit the use of other hemostasis modalities:
EVL: Endoscopic elastic band ligation GAVE: gastric vascular dysplasia EUS: Super GI endoscopy: Gastrointestinal RFA: Electrocautery ESD: Endoscopic submucosal dissection OTSC: Endoclip at the end of the bronchoscope. Injection of hemostatic epinephrine and endoclip with hemostatic forceps According to the Cochrane review, combination therapy is associated with a significant reduction in the risk of bleeding, surgery, and mortality in peptic ulcers with active bleeding. extreme or high-risk signs such as blood clots. Through the laparoscope, endoclips have been found to be effective and safe mechanical hemostatic devices when applied precisely as monotherapy or in combination. The forceps grasps the submucosal vessel, sealing the defect in the target vessel with or without approximating the sides of the lesion. Furthermore, tissue damage is minimal with clips and ulcer healing is unhindered. Introduced in clinical practice in the 1990s, over the years, the endoclip has evolved in functionality (such as accuracy, tensile strength, rotation, overshoot, and closure strength). ), physical characteristics and cost.
4. Endoscopic hemostasis injection technique
Endoscopic suture system and clamp with OTSC Clip. Mechanical methods of hemostasis have been shown to be more effective in hemostasis than injection or thermal methods alone. The OTSC clamp (Over the scope Clip, Ovesco Endoscopy GmbH, TÜbingen, Germany) is a new endoscopic cutting device that has been approved by the Food and Drug Administration. The use of the OTSC system was first reported in 2007 by Kirschniak et al. to estimate gastrointestinal tissue. Since then, this device has been widely used to control gastrointestinal bleeding, especially due to large ulcers and fibrosis at anatomical sites that are difficult to treat with transnasal forceps (TTS) or risk of perforation. Other applications include closing holes and fistulas.
The OTSC ® System Kit includes a snap cover with a metal clip, thread, thread take-up and a wheel for clamp release. The clamp is made up of a super-elastic nitinol alloy, provided with a snap cap and released by tightening the thread with a handwheel. The OTSC cap is available in 3 diameters (11, 12 and 14 mm) and 2 working depths (3 and 6 mm). There are three versions of the OTSC (trauma, trauma and more gastric wall closure clamp). Due to its unique design and elastic properties, the nitinol clamp is self-closing and ensures effective treatment by applying continuous circumferential compression sufficient to stop bleeding due to large tissue and vascular defects.

5. Techniques for using OTSC
Endoscopic ultrasound guided therapy for arterial occlusion. Endoscopic ultrasound (EUS), guided embolization with doppler monitoring of vascular response is a promising modality for the management of bleeding lesions inaccessible or difficult to access with endoscopic techniques. and standard interventional scintigraphy. EUS can detect vascular lesions in the gastrointestinal tract that are not visible to the eye during endoscopy and target lesions for injection of therapeutic agents with fine needles. Although most reports of EUS-guided arterial therapy involve variants, this technique has also been described for the management of varicose-induced upper gastrointestinal bleeding lesions. . Although the feasibility and clear safety of EUS arterial therapy have been demonstrated, the use of EUS as an interventional tool in the management of gastrointestinal bleeding remains limited in some centers. centers around the world. This is due to a lack of endoscopic training expertise and limited ability to deliver EUS in the acute care setting.
Endoscopic ultrasound (EUS) technique - Doppler guided embolization. A case of gastric aneurysm varices successfully occluded by endoscopic ultrasound
In summary, varices-associated upper gastrointestinal bleeding continues to be a persistent challenge despite advances in both pharmacological and endoscopic techniques. Several new modalities as well as modifications to traditional treatment modalities have clearly shown promise in improving outcomes whether used as monotherapy, adjuvant therapy or therapy. rescue for the management of upper gastrointestinal bleeding due to varicose veins. Because of the multiple causes of varicose veins in the upper gastrointestinal tract, the indications, efficacy, and safety of emerging endoscopic techniques continue to be determined.
In the treatment of digestive diseases, now Vinmec International General Hospital has put in modern equipment and machines to serve the examination process to bring the best treatment results for patients. patient.
In addition to quality medical facilities, the examination and treatment process is always performed by a team of qualified doctors who are trained in domestic and foreign environments. Therefore, customers can completely trust the results of the examination at the hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Alzoubaidi D, Lovat LB, Haidry R. Management of non-variceal upper gastrointestinal bleeding: where are we in 2018? Frontline Gastroenterol. 2019;10:35-42. [PubMed] [DOI] Luo PJ, Lin XH, Lin CC, Luo JC, Hu HY, Ting PH, Hou MC. Risk factors for upper gastrointestinal bleeding among aspirin users: An old issue with new findings from a population-based cohort study. J Formos Med Assoc. 2019;118:939-944. [PubMed] [DOI] Van Leerdam ME. Epidemiology of acute upper gastrointestinal bleeding. Best Pract Res Clin Gastroenterol. 2008;22:209-224. [PubMed] [DOI] Maliha Naseer et al., Endoscopic advances in the management of non-variceal upper gastrointestinal bleeding: A review, World J Gastrointest Endosc. Jan 16, 2020; 12(1): 1-16