This is an automatically translated article.
In February 1957, a new influenza A (H2N2) virus emerged in East Asia, causing a pandemic in Asia. The first cases of infection were in Singapore in February 1957, Hong Kong in April 1957, and in coastal cities in the United States in the summer of 1957. The estimated death toll was 1.1 million worldwide. and 116,000 people in the United States.
1. H2N2 . virus
The H2N2 virus is a subtype of influenza A virus. H2N2 has mutated into many different strains including the Asian flu strain, H3N2, and various strains found in birds. The H2N2 virus was also suspected of causing a human pandemic in 1889. The geographical spread of the Russian flu in 1889 was studied and published.
The Russian flu of 1978 was caused by the H2N2 virus, but no evidence was given. This was the earliest influenza pandemic with a detailed record.
Asian flu was an influenza pandemic of influenza group A that originated in China in early 1956 and lasted until 1958. Some authors believe that this virus originated from mutations in wild ducks combined with strains pre-existing human viruses.
The H2N2 virus was first detected in Guizhou, China, then it spread to Singapore in February 1957, to Hong Kong in April and the United States in June. The number of deaths in the US is about 69,800 and estimated Worldwide deaths caused by this pandemic vary widely. And it ranges from 1 to 4 million. However, according to the WHO report, about 2 million.
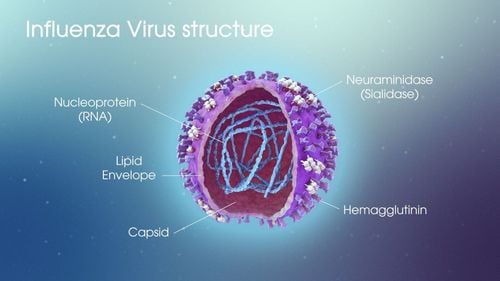
Asian flu belongs to the H2N2 subtype (symbol related to the hemagglutinin and neuraminidase protein structure in viruses) of influenza A, and the influenza vaccine was developed in 1957 to prevent its outbreak.
The Asian flu strain then evolved through antigenic transfer to H3N2, causing a milder pandemic from 1968 to 1969. Both the H2N2 and H3N2 pandemic strains contained RNA fragments of avian influenza viruses. .

Đại dịch bắt nguồn từ virus H2N2 - một chủng virus cúm A
2. The 1957 H2N2 virus pandemic
After the influenza pandemic of 1918, influenza returned to a regional pattern of lower virulence in the 1930s-1940s and early 1950s. With the first virus isolation from humans in 1933 , speculation began about a possible role for a similar virus in 1918.
However, believing that this might have been the case was difficult until the 1957 pandemic. This was the first time such an outbreak had occurred. The rapid global spread of a modern influenza virus is available for laboratory investigation. Except for people over 70 years old, most people have faced a virus without experience and knowledge about this virus.
2.1. First recognition of a pandemic In 1957, worldwide influenza surveillance was less common than it is today. However, investigators in Melbourne, London, and Washington, D.C. all soon focused on viral infections in their labs after recognizing the first serious problems with the disease.
This was followed by a 1957 New York Times publication that described the epidemic in Hong Kong with the participation of 250,000 people in a short time. Three weeks later, a virus recovered from the outbreak and was sent to the Walter Reed Army Research Institute in Washington DC for study.
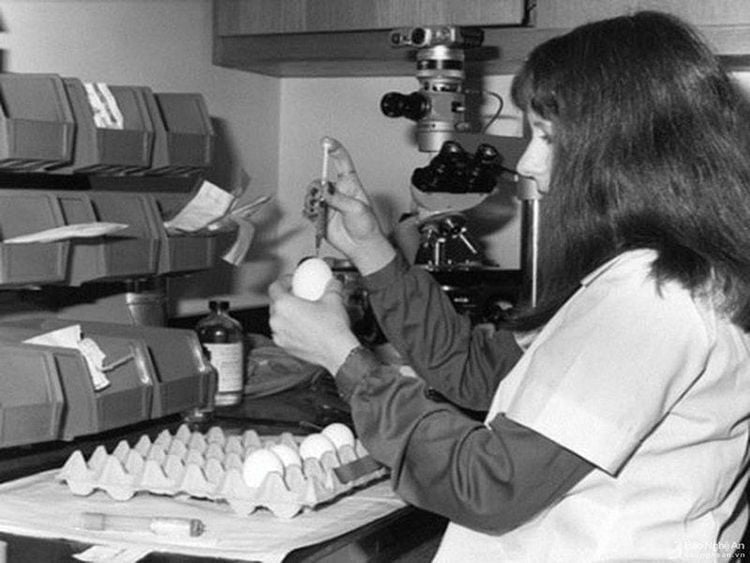
Nghiên cứu đầu tiên về đại dịch được tiến hành năm 1957
2.2 Nature of the virus The virus was quickly recognized as an influenza A virus by additional immobilization tests. However, tests that identified the virus's HA antigen showed it was unlike any previously found in humans. The same is true for neuraminidase (NA) antigen. The final type of the Asian virus was later established as H2N2.
This new virus has high sialidase/neuraminidase activity and is more stable than previous strains. Different Asian virus strains also have marked differences in their sensitivity to neutralizing antibodies or nonspecific inhibitors of hemagglutination.
In animal studies, the new H2N2 viruses did not differ in their virulence profile from the previous influenza A subtype. Virus isolates from the lungs of infected patients and fatal cases showed no significant difference from patients from throat lavage isolates with patients without pulmonary involvement during the outbreak. small.
2.3. Primary Viral Pneumonia Although secondary or concurrent lung infections were both found to be the predominant feature of deaths in 1918 when a specific etiological agent was sought. Many cases of rapid death and pulmonary consolidation or pulmonary edema occurred in which infection was not demonstrated. Because influenza persists as an endemic disease with regional recurrences after the pandemic.
With the arrival of Asian influenza A in 1957, the number of pandemic-related illnesses once again brought primary influenza virus pneumonia to the attention of hospital physicians. Contrary to observations in 1918, underlying chronic disease of the heart or lungs was found in most of these patients. Although, the deaths of formerly healthy people are not uncommon.

Virus cúm nguyên phát gây ra các hiện tượng viêm phổi
2.4. The nature of post-pandemic H2N2 infections The experience of influenza in Asia provides the first opportunity to study how post-pandemic infection and epidemic become endemic. The study was conducted in separate populations and populations, the populations being compared were Navajo School students and New York City Medical students. Results showed that in both groups, subclinical infections occurred every year during the 3-year study period and clinically manifest infection was associated with increased H2N2-specific hemagglutination inhibitory antibodies.
The reduced rate of clinically manifest cases can be attributed to an increase in antibody levels in the community or to a change in the intrinsic virulence of the virus. Therefore, the nature of the disease during the endemic period is important to determine.
A 1960 study in hospitalized patients with laboratory-confirmed infections demonstrated a range of illnesses from uncomplicated 3-day illnesses to fatal pneumonia, all of which did not There is a clear outbreak of influenza in the community. The Asian virus (H2N2) is destined to be short-lived in the human population and disappear only 11 years after it appeared. But it was replaced by the new virus in Hong Kong (H3N2).
Articles refer to sources: cdc.gov, NCBI