This is an automatically translated article.
Non-Hodgkin lymphoma is a malignant cancer that begins in the lymphatic system - part of the body's immune system. Non-Hodgkin's lymphoma occurs when lymphocytes multiply uncontrollably, producing cancer cells that have an abnormal ability to invade tissues throughout the body. The risk of non-Hodgkin lymphoma increases with age and is more common in men than women.
1. What causes non-Hodgkin lymphoma?
Researchers have found that non-Hodgkin lymphoma is associated with several risk factors, but the exact cause of the disease is not known. Determining the cause of this disease is complicated by the fact that lymphomas are a diverse group of cancers.
1.1 Changes in Genes Scientists have made great progress in understanding certain changes in DNA that cause normal lymphocytes to become lymphoma cells. DNA is the cellular component that makes up our genes, which help control how the cell works. We look like our parents because they are the source of the DNA in the body. But DNA doesn't just affect appearance, some genes control when cells grow, divide and die:
Genes that help cells grow, divide and survive are called oncogenes (oncogenes). ). Genes that help keep cell division under control or cause cells to die at the right time are called tumor suppressor genes. Cancer occurs due to DNA mutations that alter genes or inhibit genes, inhibiting tumors.
Some people receive a mutated DNA gene from one parent that increases their risk of certain types of cancer. A family history of lymphoma (Hodgkin lymphoma, non-Hodgkin lymphoma) seems to increase the risk of the disease.
However, most of the genetic changes associated with non-Hodgkin lymphoma are acquired during life, rather than inherited from parents. These acquired genetic changes can result from exposure to radiation, cancer-causing chemicals, or infections, but most often these changes occur for no apparent reason. This change is more common as the body ages, which helps explain why most lymphomas are more common in older people.
Several genetic variations leading to lymphoma are now known. For example, in follicular lymphoma, cells have an exchange of DNA (called a translocation) between chromosomes 14 and 18, which activates the oncogene BCL-2. This oncogene prevents cells from dying at the right time, leading to lymphoma.
Scientists are still learning about the exact genetic variation associated with different types of non-Hogkin lymphoma, with the aim of developing more precise tests to detect and classify certain types. lymphoma.
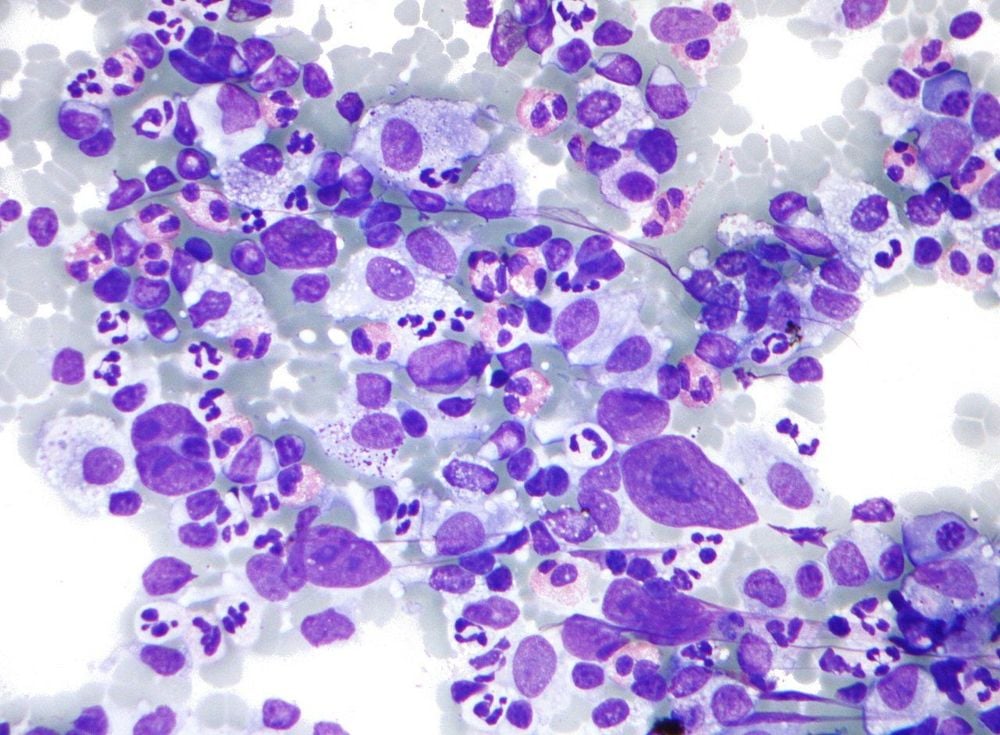
Bệnh u lympho ác tính xảy ra khi các bào bạch cầu lympho nhân lên không kiểm soát
People who are immunocompromised (due to genetics, treatment with certain drugs, organ transplants, or HIV infection) have a much higher risk of developing non-Hodgkin lymphoma than people without the system. weakened immune system. People with certain autoimmune diseases (in which the immune system repeatedly attacks a certain part of the body) have a higher risk of lymphoma. People with certain chronic infections are also at higher risk, possibly because the immune system is constantly making new lymphocytes to fight infections, which increases the likelihood of mistakes in the DNA.
2. Risk factors for non-Hodgkin lymphoma
A risk factor is anything that increases your chances of getting a disease like cancer, different diseases have different risk factors. Some risk factors, like smoking, can be changed. Other factors such as age or family history cannot be changed.
However, having one risk factor, or even multiple risk factors, does not mean you will get the disease. And many people, despite having the disease, may have few or no known risk factors.
Researchers have found several factors that may affect the risk of non-Hodgkin lymphoma.
2.1 Older adults Older adults are a high risk factor for lymphoma in general, with most cases occurring in people age 60 and older. However, there are certain types of lymphoma that are more common in young people.
2.2 Gender In general, the risk of non-Hodgkin lymphoma is higher in men than in women, but there are certain types of non-Hodgkin lymphoma that are more common in women. The exact cause for this risk factor remains unclear.
2.3 Race, ethnicity, and geography In the United States, whites are more likely to develop non-hodgkin's lymphoma than African-Americans and Asian-Americans.
Worldwide, non-Hodgkin's lymphoma is more common in developed countries, with the US and Europe having the highest rates. Certain types of lymphoma are associated with certain infections, which are more common in some parts of the world.
2.4 Family history Having a first-generation relative (parent, child, sibling) with non-Hodgkin lymphoma increases the risk of developing the disease.
2.5 Exposure to certain chemicals and drugs Some studies have hypothesized that chemicals such as benzene, herbicides, and insecticides increase the risk of non-Hodgkin lymphoma.
Some chemotherapy drugs used to treat other cancers can increase your risk of developing non-Hodgkin lymphoma years later. For example, patients who have been treated for Hodgkin lymphoma have a higher risk of later developing non-Hodgkin lymphoma. However, it is not clear whether this non-Hodgkin lymphoma is related to Hodgkin lymphoma itself or if it is an effect of chemotherapy.
Drugs used to treat rheumatoid arthritis, such as methotrexate and tumor necrosis factor (TNF) inhibitors, increase the risk of non-Hodgkin lymphoma. In fact, it is difficult to determine if this drug increases the risk because people with rheumatoid arthritis, which is an autoimmune disease, have a higher risk of developing the disease than others.

Khi tiếp xúc với một số hóa chất và thuốc làm tăng nguy cơ mắc bệnh u lympho ác tính
Patients treated with radiation therapy, such as Hodgkin lymphoma, have a slightly increased risk of developing non-Hodgkin lymphoma later in life. The risk is increased for patients treated with both radiation and chemotherapy.
2.7 Weakened Immune System People with a weakened immune system are at increased risk for non-Hodgkin lymphoma. Such as:
Organ transplant recipients are treated with drugs that suppress the immune system to prevent it from attacking the new organ. These people have a higher risk of developing non-Hodgkin lymphoma. The human immunodeficiency virus (HIV) weakens the immune system, increasing the risk of disease. In some genetic syndromes such as Wiskott-Aldrich syndrome, children are born with a weak immune system. In addition to an increased risk of serious infections, this child is also at increased risk for non-Hodgkin lymphoma. 2.8 Autoimmune diseases Autoimmune diseases such as rheumatoid arthritis, systemic lupus erythematosus, Sjogren's syndrome, and celiac disease are associated with an increased risk of the disease.
In autoimmune diseases, the immune system mistakes the body's tissues as foreign and attacks them. Lymphocytes are part of the body's immune system. The overactive immune system in autoimmune diseases causes lymphocytes to grow and divide more often than normal, increasing the risk of them developing into cancer cells.
2.9 Certain infections Certain infections increase the risk of non-Hodgkin lymphoma in different ways.
Infections that directly transform lymphocytes Some viruses can directly affect the DNA of lymphocytes, helping to transform them into cancer cells:
Infection with human T-cell lymphotropic virus (HTLV-1) increases the risk of human T-cell lymphoma. This virus is most common in some parts of Japan and the Caribbean, but they are still found around the world. HTLV-1 is spread through sex and blood, and is passed on to babies through breast milk. Epstein-Barr virus (EBV) infection is an important risk factor for Burkitt lymphoma in some parts of Africa. In developed countries, EBV is often associated with lymphomas in people with HIV infection. Human Herpes Virus 8 (HHV-8) can infect lymphocytes, leading to the rare type of effusion lymphoma. This lymphoma is most common in HIV-infected patients. Infections that weaken the immune system HIV infection weakens the immune system. HIV infection is a risk factor for several types of non-Hodgkin lymphoma, such as primary CNS lymphoma, diffuse large B-cell lymphoma, and Burkitt lymphoma.
Một số loại virus có thể ảnh hưởng đến bệnh u lympho ác tính
Infections cause chronic immune stimulation Long-term infections increase the risk of lymphoma by forcing the immune system to stay active. As more lymphocytes are made to fight infection, there is a greater chance of mutations in important genes, which can eventually lead to lymphoma. This infection-associated lymphoma usually gets better when the infection is treated. Helicobacter pylori, a bacterium known to be a risk factor for gastric ulceration, has been associated with gastric mucosal-associated lymphoid tissue (MALT) lymphoma. Chlamydophila psittaci is a bacteria that causes a lung infection called psittacosis. Chlamydophila psittaci is associated with MALT lymphoma in the tissues around the eye. Campylobacter jejuni infection is associated with a type of MALT lymphoma called immunoproliferative small intestinal disease IPSID. Long-term hepatitis C virus (HCV) infection appears to be a risk factor for lymphomas, such as splenic marginal lymphoma. 2.10 Overweight, obesity Several studies have suggested that being overweight or obese may increase the risk of non-Hodgkin lymphoma. In all cases, maintaining a healthy weight and being physically active; following a healthy diet that includes plenty of fruits, vegetables and whole grains, limiting or avoiding red and processed meats, sugary drinks and processed foods; brings many health benefits to the body.
2.11 History of breast implantation Some women with breast implants develop a rare type of lymphoma of the breast, undifferentiated large cell lymphoma. However, the risk of developing this disease after implantation is very small. This type of lymphoma is usually treated with simultaneous surgical removal of the tumor and the breast pocket.
Early cancer screening is considered a perfect measure in the timely detection and treatment of all types of cancer. Reduce the cost of treatment and especially reduce the mortality rate in patients. Vinmec International General Hospital always deploys and introduces to customers a HIGH-TECH CANCER CHECKLIST PACKAGE to help with gene testing, imaging, and biomarkers for early tumor detection. Vinmec International General Hospital has many packages of early cancer screening.
Only one gene test can assess the risk of 16 common cancers in both men and women (lung cancer, colorectal cancer, breast cancer, pancreatic cancer, neck cancer) uterus, stomach cancer, prostate cancer,....) Early detection of early signs of cancer through imaging, endoscopy and ultrasound. The operation is simple, careful and accurate. A team of well-trained specialists, especially in oncology, are capable of handling cancer cases. With facilities, advanced and modern medical equipment and a team of doctors with deep expertise and experience. At Vinmec, the examination process becomes fast with accurate results, saving costs and time for patients.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.