This is an automatically translated article.
The article was professionally consulted by Specialist Doctor I Tran Cong Trinh - Radiologist - Radiology Department - Vinmec Central Park International General Hospital. The doctor has many years of experience in the field of diagnostic imaging.Epidural hematoma is an emergency condition, the patient needs to go to the hospital quickly so that the doctor can check for signs of hematoma, symptoms of trauma, level of consciousness and increased intracranial pressure. Tests that help diagnose an epidural hematoma include blood tests, a CT scan of the head, and an X-ray.
1. Diagnostic criteria for epidural hematoma
In general, to screen for complications of epidural hematoma, it is necessary to investigate some of the following criteria:Having head trauma There is a awake interval The awake interval is the time when the patient is completely awake from the time of the accident to the time of the accident. when comatose. The shorter the waking interval, the worse the prognosis. About 60-70% of simple epidural hematomas have a clear interval, appearing from a few hours to a few days, sometimes lasting for weeks, or within 15-20 minutes. The time of onset of consciousness depends on the volume and location of the hematoma. When there are accompanying lesions, the province is almost not clear.
1.1. In case there is a craniofacial fissure on the radiograph
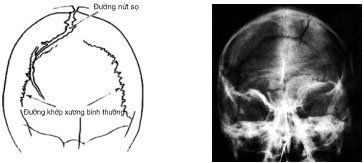
Hình ảnh nứt sọ chụp X-Quang
1.2. In case of persistent headache, even though pain relievers have been used, it is not effective. The epidural hematoma has a small volume (about 30g) in the forehead, parietal lobe or temporal lobe. Very few cases of hematoma appear in focal neurological signs, also rarely with dilated pupils. The most common symptom in patients is headache. Epidural hematomas in children rarely present with focal neurological signs, but headache is a valuable suggestion.
1.3. Occasionally, focal neurological signs are present. An epidural hematoma due to rupture of a branch of the meningeal artery will form a large mass in the temporal or central sulcus. This condition affects focal nerves, such as weakness or paralysis of the contralateral hemiparesis, sometimes with dilated pupils on the same side of the lesion. Hematomas in the temporal lobe can easily cause temporal lobe brain recession.

Tình trạng máu tụ ngoài màng cứng do đứt một nhánh động mạch màng não có thể dẫn tới bị liệt nửa người
2. Diagnostic procedure for epidural hematoma
Doctors and nurses will check the patient's level of consciousness, look for signs of arm or leg weakness, and examine the eyes to determine if there is increased intracranial pressure.2.1. Ask about the illness Time of the accident Accident circumstances (fixed or mobile head) Changes in consciousness immediately after the accident (vomiting, convulsions, reflux,...) Medical history 2.2. Consciousness disorders Assessment of consciousness according to the Glasgow scale, including the ability to open eyes, answer questions and move on command. The highest is 15 points and the lowest is 3 points, if the GLASGOW score decreases by 2 points or more, the perception worsens.
Note, the Glasgow scale does not apply to drunk people, psychopaths, taking sedatives and children under 5 years old.
2.3. Focal neurological signs

Giãn đồng tử cùng bên bị tổn thương, tăng dần là dấu hiệu thần kinh khu trú
Pupils: Dilated pupils on the affected side, gradually increasing Motor paralysis: Hemiplegia on the opposite side of the lesion May have nystagmus or hemiparesis In addition , some other signs such as the patient's coma, peripheral nerve palsy, loss of smell, strabismus, loss of vision...
2.4. Autonomic signs Common when the condition is severe, with high risk of death, including:
Increased blood pressure with increased intracranial pressure Pulse gradually decreases when there is intracranial compression Fast or slow breathing, irregularly Increase body fever, antipyretic drugs are not effective. 2.5. Laboratory tests Blood tests Blood tests may also be performed to detect clotting problems, as well as to look for other causes of confusion and/or loss of consciousness.
X-rays The victim may also need imaging of other organs or x-rays, depending on the suspected injury. For example, the doctor will order a neck X-ray to rule out other types of neck injuries. An unprepared skull X-ray helps to identify the fracture line, orient the hematoma, especially the fracture line in the temporal region.
Computed tomography has value in diagnosing and monitoring the progression of an epidural hematoma without clinical manifestations.

Xét nghiệm máu giúp phát hiện các vấn đề đông máu
3. CT Scan - the gold standard in diagnosing epidural hematoma
CT Scan plays an important role, helping neurosurgeons answer 5 diagnostic criteria, and monitor intracranial complications, especially epidural hematoma. Biconvex lens image, close to the skull bone, hyperattenuated, homogeneous and localized (does not exceed the joints). The hematoma can compress surrounding brain tissues, midline, and ventricular system.Large epidural hematoma in the frontal region and prolonged compression of the anterior cerebral artery group can lead to sub-crescent brain recession, cerebral edema and cerebral ischemia. The occipital epidural hematoma has few focal neurological signs, but if it grows too large, it will cause ischemia, and when the cerebral edema spreads to the inner capsule, there will be focal neurological signs.
While a headache at the superior site is an early sign, an epidural hematoma in the posterior fossa often causes an early increase in intracranial pressure. Lesions in this area push the fourth ventricle, or block the foramen of Magendie and Luschka, leading to ventricular dilation and cerebellar amygdala. The most obvious manifestation is a headache, often severe in the occipital and suboccipital regions, especially in young children who scream loudly due to overstimulation of the meninges. Only about 20-30% of these lesions show cerebellar signs.
Cranial angiography in the TOWNE position is essential to find occipital and suboccipital craniofacial fissures, but to screen for epidural hematomas, a CT Scan of the head without contrast medium is a very effective method. In addition, cerebral angiography by Seldinger method also helps to detect epidural hematoma, but the value is not high. This method is only indirectly evaluated through the change in the position of the cerebral arteries in the posterior fossa and requires a lot of experience.
Epidural lesions can appear in two locations on the same side or on both sides. However, the encephalogram is difficult to detect two different locations at the same time, only CT Scan helps diagnose the most accurate epidural hematoma.
In cases where an epidural hematoma occurs at the same time as a subdural hematoma or a superficial cerebral contusion - especially a small lesion, it is easy to miss a subdural hematoma by CT Scan.
In general, head CT scans are good at detecting intracranial epidural hematomas, as well as showing skull fracture if traumatic brain injury is present. The definitive diagnosis of epidural hematoma will be based on clinical manifestations and computed tomography images.
Currently, Vinmec International General Hospital is equipped with a 640-slice CT scanner TSX - 301C manufactured by Toshiba capable of supporting diagnosis on an area of up to 16cm wide, fast speed for accurate and clear images. strokes. In particular, this machine can reduce up to 90% of radiation dose, so it can be taken for pregnant women when indicated.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.