The development of antibiotic-resistant bacteria
In recent years, antibiotic resistance has skyrocketed and has even become an alarming problem. Most antibiotics if not effective, will affect the treatment process and the patient's health.
1. Alarming numbers of antibiotic resistance
In the past, most doctors underestimated the concept of "antibiotic-resistant bacteria" because at that time, prescribing antibiotics for patients was still very effective. However, in recent years, this problem has become alarming.
The types of bacteria have changed and become inactive to antibiotics. This is due to the fact that antibiotic prescriptions are prescribed indiscriminately, people can even buy antibiotics arbitrarily at any pharmacy. The widespread and pervasiveness of antibiotics in everyday life has been causing new strains of bacteria to emerge stronger.
According to sugar records, antibiotic resistance is increasing and reaching dangerous levels in all countries of the world. All infections are becoming harder to control/treat than ever before because antibiotics can no longer inhibit them.
WHO says: Every minute, there are... 19 deaths due to antibiotic resistance. This situation also places a heavy burden on the economy worldwide. Every year, hundreds of billions of dollars are spent to control the number of deaths due to drug resistance as well as to research new antibiotics.
More specifically, every year, up to 800 million USD is used to research new antibiotics for pulmonary tuberculosis, but within 50 years, only 2 antibiotics have been developed, but still in the early stages. test segment. Not stopping there, antibiotic resistance is a threat to the health of all people around the world. These pathogenic bacteria, if no measures are taken, they will very quickly grow and develop.
A report from ECDC (European Center for Disease Prevention and Control) said: In Europe, every year up to 25,000 patients die from multidrug-resistant strains of bacteria. Each year, these types of bacteria increase 6 times.
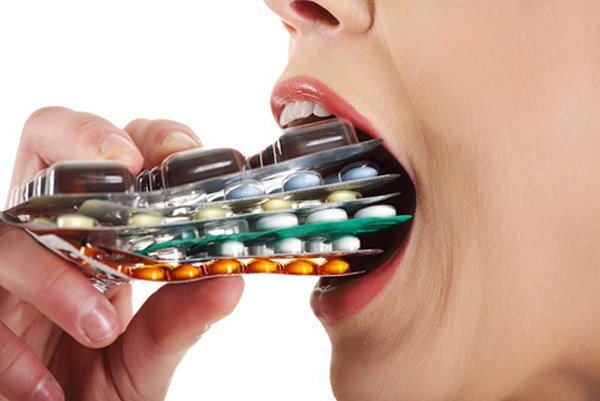
Tình trạng lạm dụng thuốc kháng sinh đang diễn ra ngày càng phổ biến
2. How do antibiotic-resistant bacteria form?
What are resistant bacteria (or antibiotic-resistant bacteria) and why can they be resistant to drugs? This is a question that many scientists conduct research. Since then, the formation of these drug-resistant bacteria is mainly based on the following 3 mechanisms:
Limiting the penetration of antibiotics All types of bacteria have their own solutions to limit the invasion from antibiotics into the cell. This restriction will become stronger and more effective through many attacks. Therefore, antibiotics will gradually have less opportunity to affect and kill bacteria.
To do this, bacteria actively increase the stability of the protective membrane (such as the outer gills in gram-negative bacteria) or can also use the push-pull mechanism inside the cell to push the antibiotic invade outside (occurs in blue pus bacilli, Acinetobacter...).
In other words, they will put on a sheet of "armor" or push the antibiotic out with great force, making the antibiotic less likely to kill them.
Destroying antibiotics Some other groups of bacteria will choose to secrete enzymes to destroy antibiotics. This phenomenon occurs very clearly in intestinal bacteria, Staphylococcus aureus.
In Staphylococcus aureus, the enzyme that destroys them is synthesized Beta-Lactamase. This enzyme breaks the lactam ring bond of the antibiotic.
In intestinal bacteria such as Klebsiella sp, E.coli... Broad-spectrum Beta-lactamase enzyme will be synthesized. This enzyme is resistant to most current lactam antibiotics (except for a few new ones).
More specifically, recently, bacteria have been able to synthesize NDM-1 with the function of resistance to all antibiotics. This is a particularly serious condition that marks the overgrowth of bacteria.
It can be said that, if encountering antibiotics strong enough to penetrate their defenses, bacteria will actively secrete chemicals to destroy antibiotics.
Antibiotic inactivation This is the last mechanism of antibiotic resistance discovered recently. Bacteria can block or modify the targets of antibiotics on their own cells, thereby causing ineffective drug. This phenomenon comes from a mutation in the chromosome (or plasmid) of the bacterial cell.
This mechanism usually occurs in gram-positive cocci (eg, Staphylococcus aureus or Streptococcus pneumonia) and very rarely in gram-negative bacteria.
Mutations in bacteria's genes will make antibiotics no longer able to inhibit their growth.
3. Facing the battle against antibiotic-resistant bacteria, what to do?

Để tránh tình trạng kháng kháng sinh xảy ra, mọi người nên sử dụng thuốc kháng sinh một cách hợp lý, an toàn
The overuse of antibiotics is the cause of today's alarming antibiotic resistance. Therefore, in order to protect themselves and those around them, or even more globally, each person needs to be aware of:
Use antibiotics in a rational and scientific way, absolutely do not abuse drugs. Only use antibiotics when you are sure you have an infection. After the indicated course, it is necessary to stop the use of antibiotics immediately. However, it should not be stopped early even if there are no signs of illness. Each type of antibiotic will have a different target of bacteria that need to be destroyed. Choose the right antibiotic, do not use it arbitrarily or indiscriminately. It can be said that antibiotic-resistant bacteria has become a global concern. Therefore, in order to limit antibiotic resistance and future generations do not have to suffer great consequences from these bacteria, you need to have a sense of using antibiotics correctly and scientifically.
SEE ALSO:
Antibiogram - solutions to reduce antibiotic resistance When should antibiotics be stopped? How to limit antibiotic resistance?






