This is an automatically translated article.
Esophageal compression is an abnormal narrowing of the esophagus, causing difficulty swallowing and choking. This condition has many potential causes, sometimes due to esophageal tumors or external influences. At this time, upper gastrointestinal endoscopy is often the first diagnostic modality indicated, helping to find the cause of esophageal compression and allowing for proper therapeutic intervention.
1. Why is there esophageal compression?
In most cases, the cause of esophageal compression is usually:
Progression of esophageal trauma; Local or extrinsic tumor growth; Presence of food and foreign bodies. Esophageal injuries that progress to esophageal compression or obstruction may be caused by damage to the esophagus with repeated reflux of acid from the stomach (gastroesophageal reflux), often over many years. Esophageal obstruction can also be caused by damage to the esophagus that occurs after swallowing a corrosive substance (erosive esophagitis) or occurs after the esophagus becomes inflamed due to a pill that has been stuck in the esophagus for a long time. .
In addition, esophageal tumors are a serious cause of esophageal compression, including cancerous and noncancerous tumors of the esophagus.
Furthermore, esophageal compression can also occur when something presses on the esophagus from the outside. There are several causes to consider, such as:
Dilation of the left atrium of the heart with mitral stenosis; Aortic aneurysm; Abnormally formed blood vessels; Abnormally large thyroid gland; Bones grow from the spine; Cancer (most commonly lung cancer). Sometimes the cause of esophageal compression is genetic. These disorders usually cause only partial esophageal obstruction.
Because all of these conditions reduce the diameter of the esophagus, patients often present with dysphagia, choking on swallowing solid foods, especially meat and bread. Difficulty swallowing liquids will develop later.

Chèn ép thực quản có thể do khối u ung thư gây ra
2. How to diagnose esophageal compression?
When taking a medical history of dysphagia, choking persists from solid food to liquid food and esophageal stricture is suspected, the best indication for esophageal compression is always internal medicine. esophagoscopy or esophagography with contrast.
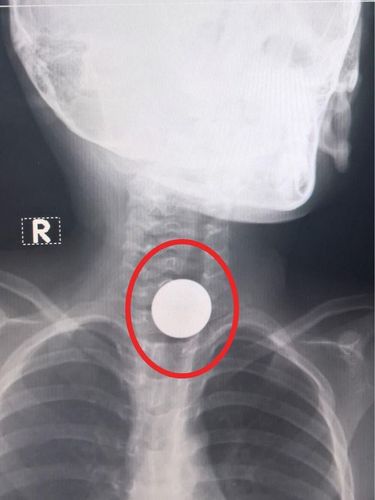
Both of these imaging methods are the primary diagnostic modality for esophageal compression. Depending on the severity of dysphagia and the presence of other clinical symptoms, a person may need a chest X-ray to evaluate for problems such as foreign body compression or diaphragmatic hernia and rule out certain other lung conditions. Sometimes, a CT scan is more helpful in patients with a history of erosive ingestion to detect esophageal perforation. However, X-rays and CT scans are not needed in routine cases. CT will become more useful in patients who are found to have malignancy at biopsy and help with staging.
Most patients are evaluated endoscopically because it can provide comprehensive information about the esophageal anatomy and confirm the diagnosis, allowing mucosal biopsies. Endoscopy offers the opportunity to treat muscle relaxation when indicated. Contrast endoscopy is reserved for patients with complicated compression esophageal stricture or when endoscopy is incomplete due to excessive compression of the lumen. Usually, the physician uses a water-soluble contrast medium for the first look to avoid the development of heavy agents such as barium, to minimize the risk of obstruction and/or the need to aspirate fluid from the esophagus.
3. How to treat esophageal compression?
There are different methods and tools used to achieve esophageal compression and improve circulation in the esophageal lumen. Treatment includes the use of an esophageal sphincter relaxant, stenting, and surgical removal of the esophagus.
Among them, the most commonly used and benign technique is endoscopic dilation of the esophagus using a balloon or a balloon dilatation device. The main goal is to improve symptoms, mainly to relieve dysphagia, choking for the patient.
Interventional esophageal stenting, against esophageal compression is usually reserved for cases of esophageal tumors causing malignant and benign strictures. The goal of stenting is to keep the esophageal lumen open for a long time, while the patient is still physiologically able to eat and drink. In the case of malignant esophageal tumours, stenting can be used for complete palliation in the case of advanced cancer or temporary palliation in the case of adjuvant neoplasia.
Esophageal resection due to esophageal compression is reserved for narrowing of the esophagus caused by a group of malignancies or benign conditions that are not compatible with the above forms of conservative treatment. At this point, esophageal dilation may be necessary in cases of malignant esophageal stricture, in which resection of the tumor causing esophageal compression is also possible, if favorable. In such cases, the surgeon will remove part or all of the esophagus, pull up the stomach tube, or place a loop of bowel to reshape the upper digestive tract.
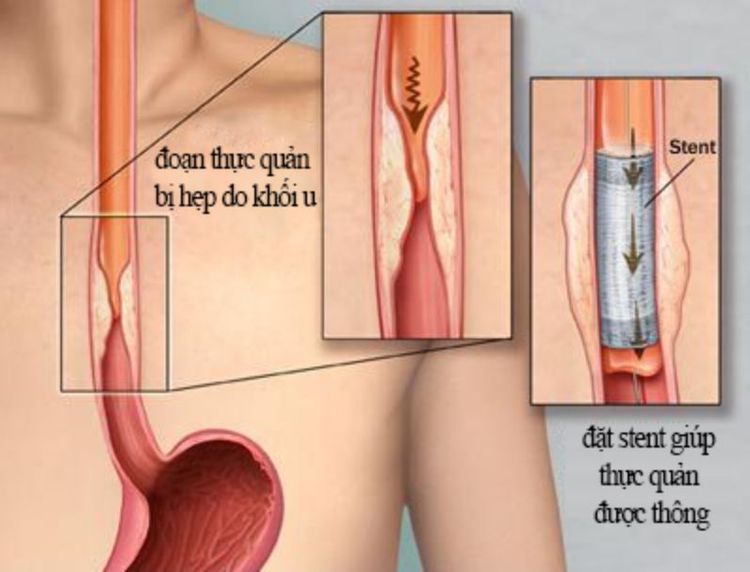
Điều trị chèn ép thực quản bằng phương pháp đặt stent thực quản
4. Complications of esophageal compression
Complications related to esophageal compression, if not diagnosed and not treated in time, will cause:
Poor appetite; Difficulty swallowing; Choking; Inhalation of food; Asthma caused by inhalation; Severe chest pain; Esophageal perforation due to long-term infection; Esophageal fistula formation. On the other hand, esophageal interventions to relieve esophageal compression also have potential risks. For example, ischemic complications from dilation and stenting can cause bleeding and perforation of the esophagus. Therefore, patients need to be guided on how to follow up after the intervention, such as re-examination immediately when symptoms of dysphagia or vomiting regurgitate.
In summary, acute esophageal compression caused by food or foreign bodies can be a medical emergency. In contrast, local esophageal tumors or external masses can compress the esophagus over time, making it difficult for patients to swallow, gradually increasing choking. Regardless of the cause, when patients receive upper gastrointestinal endoscopy for early diagnosis, the likelihood of successful treatment is high, significantly improving the long-term prognosis of the disease.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: ncbi.nlm.nih.gov, accesssurgery.mhmedical.com, winchesterhospital.org, medanta.org