This is an automatically translated article.
The thymus makes white blood cells called T lymphocytes that fight infections. And these cells play an important role as the baby's immune system develops. The thymus begins to shrink after puberty.
1. What is the thymus?
The thymus is a specialized primary lymphoid organ of the immune system. Along with the thymus are mature T cells. T cells are important for the adaptive immune system, where the body adapts specifically to external factors.The thymus consists of two identical lobes, and the thymus is located in front of the mediastinum, in front of the heart, and behind the sternum. Each lobe of the thymus can be divided into a central medulla and a peripheral cortex surrounded by an outer capsule.
The cortex and medulla play different roles in T cell development. The cells in the thymus can be divided into thymocytes and cells of hematopoietic origin (derived from bone marrow hematopoietic cells). The developing T cells are called thymic cells and are of hematopoietic origin. The stromal cells include epithelial cells of the thymus, medulla, and dendritic cells.
The thymus provides a medium for the development of T cells from progenitor cells. The cells of the thymus provide the development of functional and self-tolerant T cells. Therefore, one of the most important roles of the thymus is to induce central tolerance.
The thymus is largest and most active during infancy and pre-adolescence. By adolescence, the thymus begins to decrease in size and function. The tissue of the thymus is gradually replaced by adipose tissue. However, T-lymphogenesis continues throughout life.
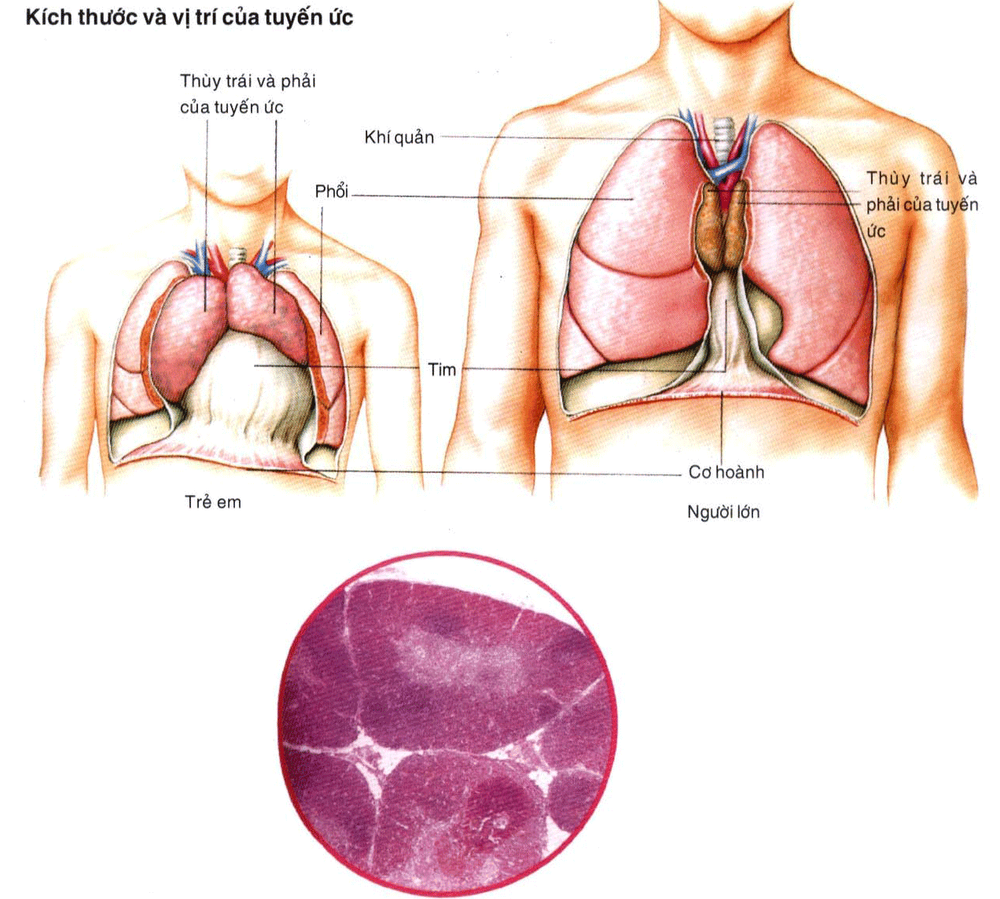
Vị trí của tuyến ức trong cơ thể
2. The role of the thymus in the endocrine system
The thymus produces progenitor cells and matures into T cells. The body uses T cells to help destroy infected or cancerous cells. The T cells produced by the thymus also help other organs in the immune system develop properly.
2.1. T-cell maturation The thymus facilitates the maturation of T cells, an important part of the immune system that helps provide cell-mediated immunity. T cells start as hematopoietic precursors from the bone marrow and migrate to the thymus, where they are known as thymus cells.
In the thymus, they undergo a maturation process that includes ensuring that the cells react against antigens (positive selection), but they do not react to antigens already found on muscle tissue possible (negative selection). After maturation, T cells migrate from the thymus to provide important functions for the immune system.
Each T cell has a distinct T-cell receptor, which matches a specific substance, called an antigen. Most T-cell receptors bind to tissue complexes mainly on the cells of the body. To function properly, a mature T cell needs to be able to bind to the MHC molecule and not react against real antigens from the body's tissues. Positive selection occurs in the cerebral cortex and negative selection occurs in the medulla of the thymus. After this process, the surviving T cells leave the thymus, which is regulated by sphinogosine-1-phosphate. This happens because of hormones and cytokines secreted by the thymus.
Tế bào T
2.2. Positive selection T cells have differentiated T cell receptors. These distinct receptors are formed by VDJ recombinant gene rearrangements stimulated by the RAG1 and RAG2 genes. This process is error-prone and some thymocytes are unable to produce functional T-cell receptors, while other thymocytes produce autoreactive T-cell receptors. If a functional T-cell receptor is formed, the thymus will initiate simultaneous expression of the cell surface proteins CD4 and CD8.
The survival and nature of the T cell then depends on its interaction with the surrounding thymic epithelial cells. Here, the T-cell receptor interacts with the MHC molecule on the epithelial cell surface. A T cell with an unresponsive or weakly responsive receptor dies. An unresponsive T cell will survive and proliferate. An adult T cell expresses only CD4 or CD8 but not both. This depends on the strength of the binding between the TCR and MHC class 1 or class 2. A T cell receptor that binds predominantly to MHC class 1 tends to produce a cytotoxic "CD8-positive T cell" cells" mature. A T-cell receptor that binds primarily to MHC class 2 tends to induce CD4-positive cells.
2.3. Negative selection T cells that attack the body's proteins are eliminated in the thymus. Epithelial cells in the marrow and dendritic cells in the thymus express key proteins from elsewhere in the body. Thymus cells are highly reactive to antigens. Some antigen-exposed CD4-positive T cells persist as regulatory T cells.
3. Diseases related to the thymus
The most common thymic diseases are myasthenia gravis (MG), pure red blood cell aplasia (PRCA), hypoglycemia according to NLM.
Myasthenia gravis occurs when the thymus gland is abnormally large and produces antibodies that block or destroy muscle receptor sites. This causes muscles to become weak and prone to fatigue.
Pure red cell aplasia is thought to be caused by the patient's own immune cells attacking the hematopoietic stem cells. This happens when the thymus has a tumor. Blood transfusions to increase red blood cell levels, corticosteroids, and immunosuppressive therapy can all be treatments for this condition.
Bệnh nhược cơ do tuyến ức
Hypoglycemia is a disorder in which the body does not produce enough antibodies.
Thymus cancer is a disease of the thymus gland, not the thymus. Symptoms may include shortness of breath (possibly with bloody sputum), chest pain, difficulty swallowing, loss of appetite, weight loss, headache, and swelling of the face and neck. Thymus cancer is treated with surgery, radiation, or chemotherapy.
Articles refer to sources: Webmd.com, Livescience.com
SEE MORE:
T-lymphocytes: What you need to know Patient U50 with multiple myeloma gets healthy thanks to hematopoietic stem cell transplantation What is a gene? What is a genetic disorder?