This is an automatically translated article.
Pain is an abnormal manifestation of the body, a common symptom in clinical practice. Pain can be divided into three types based on the cause of pain sensation: nociceptive pain, neuropathic pain, and psychological pain. In this article, we will learn more specifically about pain caused by nerve causes.
1. What is neuropathic pain?
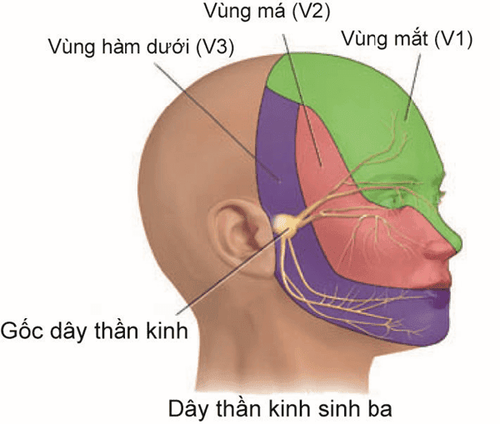
Neuropathic pain is a complex field of medicine. Neuropathic pain is an inappropriate response caused by a lesion or dysfunction in the central or peripheral nervous system.
Pain is often diagnosed as neurogenic when pain is disproportionate to tissue damage, sensory disturbances (such as burning, tingling, etc.) examination process.
Neuropathic pain may manifest itself as: pain without a stimulus (pain that is not due to painful stimuli) and or excessive pain produced after a stimulus (pain from painful stimuli).
In which, non-stimulus pain includes the following symptoms:
Burning, continuous pain; Sharp, intermittent pain that can be as painful as a shot; Pain like an electric shock; Hyperalgesia: Hyperalgesia is a state of increased response to painful stimuli in cases of stimuli below the threshold of pain. Paresthesia: abnormal sensations usually not caused by external stimuli such as ants crawling, numbness like needles, tingling or burning... Allodynia: is an abnormal sensation, not easy. bear. Pain can manifest after nerve damage to any degree. Possibly after peripheral or central nerve damage; Sympathetic nervous system involvement (prolonged pain of sympathetic origin) may be involved.
Specific syndromes include: postherpetic neuralgia (postherpetic neuralgia), radiculopathy, pain due to mononeuropathy, polyneuropathy, peripheral neuropathy, diabetic pain, postoperative pain syndromes (post-mastectomy syndrome, post-thoracotomy syndrome, phantom limb pain) and complex regional pain syndromes (sympathetic dystonia and myalgia) , pain after stroke .
2. Basic mechanism of neuropathic pain symptoms
The underlying mechanisms of neuropathic pain symptoms:
Peripheral sensitization; Displaced electrical discharge; Central sensitization; Central remodeling of Aβ fibers; Loss of inhibitory control.

Đau do nguyên nhân thần kinh là một lĩnh vực y học phức tạp
3. When is neuropathic pain diagnosed?
Clinical evaluation, neuropathic pain is suspected when symptoms are characteristic with or suspected nerve damage.
The cause is easily identifiable (eg diabetes...). Based on symptom description. Persistent pain of sympathetic etiology is improved by sympathetic nerve blockade.
4. Evaluation of neuropathic pain
Pain Scales are available tools to assess the quality, intensity, location, and pattern of pain. Prior to treatment, the same scale was used to assess and monitor the patient's response to treatment over time. Some of the commonly used tools to assess neuropathic pain are as follows:
4.1. Pain Rating Scale Pain grading scale uses words to describe pain severity or intensity. For example, pain intensity is rated on a 4-point classification scale such as: no pain ~ 0, mild pain ~ 1, pain ~ 2 and severe pain ~ 3.
4.2.Visual analogue scale [Visual analogue scale] scales (VAS)] This is one of the simplest, most commonly used scales: Patients are asked to divide their pain level on a 100mm long horizontal line (For example, 0mm is equivalent to zero). pain & 100 mm is equivalent to the most pain).
VAS is also used to evaluate the effectiveness of treatment: 0mm is equivalent to complete pain relief and 100mm is equivalent to no analgesia.
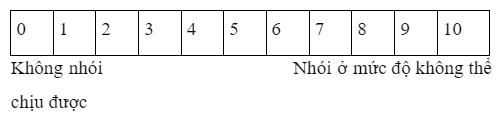
4.3. Verbal rating scales [Verbal rating scales] Similar to the VAS scale, but pain is rated on a scale of 0 to 10, (0= no pain and 10= severe pain).
4.4. McGill Pain Questionnaire (MPQ) This table includes questions that describe pain sensation, pain assessment, pain effects, along with intensity scales, and other questions. The patient completed a questionnaire including the following:
Location of pain; Describe the feeling; Pain patterns, which change over time; Rate pain intensity on a scale of 1 (mild pain) to 5 (severe). The McGill Pain Questionnaire (MPQ) is a comprehensive questionnaire for the assessment of overall pain. Therefore, it is a sensitive tool for assessing pain management. However, the questions are quite complex leading to its limited application in daily clinical practice.
4.5. The Neuropathic Pain Scale (NPS) NPS is designed to assess pain in confirmed neuropathic pain syndromes and is sensitive for assessing treatment outcome. The NPS consists of 10 questions that assess the intensity, discomfort, quality and chronology of the pain:
Some sample neuropathic pain scale questions are as follows:
Tell us Mr/ How severe is your pain?
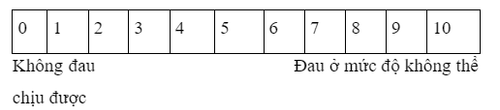
Tell us how do you feel the pain?
4.6. Patient logbook Some patients may regularly record pain episodes. This may provide a useful and reliable tool for pain assessment on a more continuous basis than the patient's recollection at examination.
4.7. Quality of Life (QoL) Scales There are many different QoL scales. The Short-form-36 (SF-36) scale is a very popular scale, often used in clinical trials. SF-36 includes 36 questions to assess 8 quality of life areas: physical activity, physical role, physical pain, mental health, emotional role, social function, markers survival and general health. The SF-36 provides a comprehensive picture of quality of life. Therefore, pain management should have a positive effect on overall quality of life.

Sử dụng thuốc là một trong những phương pháp điều trị đau do nguyên nhân thần kinh
5. How is neuropathic pain treated?
Pain due to nerve causes is often treated with a combination of methods:
Treatment of psychological factors; Physical methods, rehabilitation; Drug therapy: Antidepressants (clomipramine, imipramine, amitriptyline), anticonvulsants (gabapentin, pregabalin), topical medications such as 5% lidocaine patch may be effective for peripheral pain syndromes. Opioid analgesics can provide pain relief, but are generally less effective in acute nociceptive and side effects that interfere with adequate analgesia.
The patient can be operated on in some necessary cases. Some other potentially effective treatments include:
Spinal cord stimulation with an epidural electrode is used in certain cases of neuropathic pain (eg, chronic leg pain after spinal surgery) ). Electrodes implanted along ganglia and peripheral nerves in some chronic neuropathic pain diseases. Sympathetic nerve block in some patients with complex local pain syndromes. For pain caused by peripheral nerve damage, efforts should be made to prevent or eliminate muscle atrophy and stiffness.
During the treatment of neuropathic pain, the patient must always consider psychological factors from the beginning of treatment. Anxiety and depression must be treated appropriately. For patients whose dysfunction has become persistent, a comprehensive approach should be taken in a specialized neuro-analgesia facility.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.