This is an automatically translated article.
Arterial blood gas helps to assess the patient's acid-base balance, ventilation and oxygenation status, which is a very important test, especially for critically ill patients.
1. What is the arterial blood gas test for?
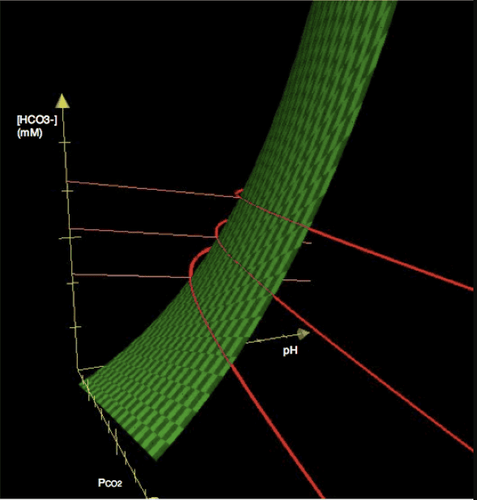
Arterial blood gas is a test done on a patient's arterial blood. The test will help provide parameters such as blood pH, arterial blood carbonic pressure (PaCO2), plasma bicarbonate concentration HCO3-, arterial blood oxygen saturation (SaO2) and partial pressure of dissolved oxygen in arterial blood (PaO2). These parameters will help the physician assess the patient's acid-base balance, ventilation status, and oxygenation status.
This information is very important in diagnosis, monitoring and treatment, especially for critically ill patients. For patients requiring mechanical ventilation, the results of arterial blood gas testing performed prior to mechanical ventilation will help to adjust ventilator parameters.

Xét nghiệm khí máu động mạch giúp chẩn đoán bệnh lý chính xác
2. How to draw blood for arterial blood gas test
To get a blood sample for testing, the medical staff will draw blood from the patient's artery. The most commonly used blood collection sites are the radial artery of the wrist, the brachial artery, and the inguinal artery. In which, drawing blood from the radial artery is the most difficult and the inguinal artery is the easiest, due to the large diameter of the inguinal artery, the diameter of the returning artery is quite small. However, in terms of safety, drawing blood from the radial artery is the safest.The radial artery is the most commonly used site in clinical practice, if the radial artery fails to draw blood, the doctor will only appoint another site to draw blood. The reason for this choice is that when the needle is inserted into the artery to draw blood, there is a risk of thrombosis and embolism, which is a very dangerous complication. In the hand, there are two arteries supplying blood, the radial artery and the ulnar artery. If a thrombus forms and completely occludes the radial artery, the ulnar artery will still be able to supply blood and the hand will not be necrotic.
Assessing the function of the ulnar artery before drawing blood is very important, to ensure that the ulnar artery is working stably and is able to supply enough blood to the hand if radial artery thrombosis occurs. The most commonly used measure is to perform the Allen test. The Allen test is performed as follows:

Cách lấy máu để làm xét nghiệm khí máu động mạch
The patient is instructed to make a fist to reduce the amount of blood entering the hand. The nurse will use the index and middle fingers to press on the path of the radial and ulnar arteries for a few seconds. The patient's hand will turn white because of the reduced blood flow to the hand. Release the finger holding the ulnar artery, if the hand is pink again in 7-10 seconds, it means that the blood is well supplied to the hand. If the hand does not return to red, indicating that the ulnar artery in that hand is not supplying enough blood to the hand, conduct an examination in the other hand.
3. Basic Arterial Blood Gas Reading
Blood gas values are normal when in the following ranges:
blood pH: 7.35-7.45 PaCO2: 35-45 mmHg HCO3-: 22-26 mEq/l SaO2: 95-100% PaO2: 80-100 mmHg Basic arterial blood gas readings follow these steps:
3.1. How to read arterial blood gas to assess acid-base status: Step 1: Compare the pH with the normal range, if pH < 7.35 indicates the patient has acidosis, if pH > 7.45, the patient is alkaline blood. However, in some cases where the disease may have a combined metabolism (concurrent acidosis and alkalosis), the patient's pH may be in the normal range.
Step 2: Identify the primary disorder leading to the pH change
Determine the changes of PaCO2 and HCO3-:
PaCO2 <35: called respiratory alkalosis PaCO2 >45: called respiratory acidosis HCO3 - <22: called metabolic acidosis HCO3- >28: called metabolic alkalosis Find the primary disorder as follows:
When the patient has acidosis (pH <7.35) and : Only In case of metabolic acidosis (HCO3- <22), the primary disorder causing changes in pH is metabolic (renal). Only respiratory acidosis (PaCO2 > 45), the primary disorder is respiratory (pulmonary). If both metabolic and respiratory acidosis are present, the primary cause of the disorder is a combination, both respiratory and metabolic. If neither metabolic nor respiratory acidosis is present, either the test is normal (pH>7.35) or the test is false. When the patient has a blood alkaline state (pH>7.45) and: Only metabolic alkalosis (HCO3- >28), the primary disorder is metabolic (renal). Only respiratory alkalosis (PaCO2 <35), the primary disorder is respiratory (pulmonary). If both respiratory and metabolic alkalosis are present, the primary disorder is caused by both respiratory and metabolic disorders. If neither metabolic nor respiratory alkalosis is present: test is false or test is normal.
Xét nghiệm khí máu động mạch
Step 3: Assess compensatory response
If the primary disorder is due to breathing, the kidneys will try to adjust HCO3- to bring the pH level back to the normal range. If the disorder is primarily metabolic, the lungs will adjust to CO2 to bring the pH back to normal. The rate of compensation varies with respect to respiratory or metabolic compensation. If there is a metabolic disturbance, then respiratory compensation will occur immediately.
For example, a patient receiving intravenous hydrochloric acid has metabolic acidosis, the patient's body will rapidly increase ventilation and produce respiratory alkalosis to bring the pH back to normal. Metabolic compensation for respiratory abnormalities will be slow and may take several days. For example, a person moving to high altitude, started to be ventilated by low oxygen concentration in the air, first there will be no metabolic compensation, blood pH will be high, after many days, metabolic compensation will occur and blood pH will be low. back to normal.
Based on the HCO3- and PaCO2 indexes, examination, comparison and clinical status, the doctor determines whether the compensation is appropriate or not and prescribes appropriate treatment.
3.2. How to read arterial blood gas to assess ventilation Ventilation assessment is based on PaCO2:
PaCO2 <35: hyperventilation PaCO2 > 45: hypoventilation 3.3. Arterial blood gas reading to assess gas exchange PaO2 is the partial pressure of O2 in the blood, which can be used to assess respiratory failure:
| PaO2 | Độ suy hô hấp |
| 79-60 | Nhẹ |
| 59-40 | Trung bình |
| <40 | Nặng |
PaO2 also helps to evaluate the effectiveness of oxygen therapy: (FiO2 indicates the percentage of oxygen in the measured volume, in nature, oxygen accounts for 20.9%, equivalent to FiO2 of 0.0209. Patients on mechanical ventilation with breathing air have high oxygen content, will have higher FiO2 than normal).
| PAO2 (mmHg) | Ý nghĩa và cách xử lý |
| <60 | Giảm O2 máu chưa được điều chỉnh nếu đã có tăng FiO2 |
| 60< PAO2<100 | Giảm O2 máu đã được điều chỉnh nhưng sẽ giảm nếu giảm FiO2 |
| 100< PAO2< PAO2 dự đoán | Giảm oxy máu đã điều chỉnh dư. |
| PAO2> PAO2 dự đoán | Sẽ giảm O2 máu nếu ngưng cung cấp O2 nhưng có thể giảm FiO2 được. |
| Giám oxy máu đã điều chỉnh quá dư, có thể không giảm O2 máu nếu ngưng cung cấp O2 .Phải giảm từ từ FiO2 |
The ratio PaO2/FiO2 is used to monitor acute respiratory failure and shunt: PaO2/FiO2 <300: the patient may be hypoxic, acute lung injury.
PaO2/FiO2 <200: the patient is in acute respiratory failure.
PaO2/FiO2 >350: patient is overoxygenated
PaO2/FiO2 between 100-500: decrease every 100 then increase shunt 5%: (500-PaO2/FiO2)x%
PaO2/FiO2 <100: decrease every 15-20% increase shunt by 5%
| <10 | Shunt bình thường |
| 10-19 | Shunt bất thường, chưa có ý nghĩa lâm sàng |
| 20-29 | Shunt đáng kể, nguy hiểm nếu tim mạch, thần kinh bất thường |
| > 30 | Nguy hiểm, điều trị hô hấp tim mạch tích cực |
| > 60 | Giới hạn cuối |

Labo xét nghiệm tại Vinmec được trang bị hệ thống máy móc hiện đại
Customers can directly go to Vinmec Health system nationwide to visit or contact the hotline here for support.
MORE:
What is respiratory acidosis? PaO2, PaCO2, FiO2 indicators in arterial blood gas test results Tests to help detect chronic obstructive pulmonary disease













