This is an automatically translated article.
Horton's disease is systemic inflammation of the arteries but is localized mainly in the temporal artery. This is a disease that causes many dangerous complications for vision, if not detected and treated promptly, the nerve cells in the retina or the optic nerve will be completely paralyzed leading to permanent blindness. far.
1. Causes and subjects susceptible to hormone disease
Systemic arteritis is common in both men and women, people over 60 years of age are more susceptible to hortoniasis, and women are more likely to have it than men.
Horton's disease is caused by an autoimmune mechanism that causes inflammation of the inner elastic layer of many arteries, especially the superficial temporal artery and branch of the external carotid artery. Through many studies, it has been determined that hormone disease is hereditary.
2. Horton disease and typical signs
2.1. Headache is a prominent symptom
Horton's disease has a characteristic and easily recognized symptom as a headache, especially headache in the temporal region. Pain in the temporal region is usually pain on one or both sides. Hormonal headaches are often persistent in nature. The patient will feel a stinging pain under the scalp, the pain starts at the temples and then spreads to the forehead, eye sockets, or the top of the head.

Người bệnh thường đau buốt từ thái dương lan ra khắp đỉnh đầu
The pain often occurs naturally or due to a very small impact on the scalp such as combing hair, wearing glasses, washing hair... The pain will increase strongly when it is cold and at night. In addition to the persistent pain, horton's disease also causes severe pain that feels like something is drilled into the temple, these paroxysmal pain will last for 2-3 hours / day, each day from 1 to 2 bouts.
2.2. Visual symptoms
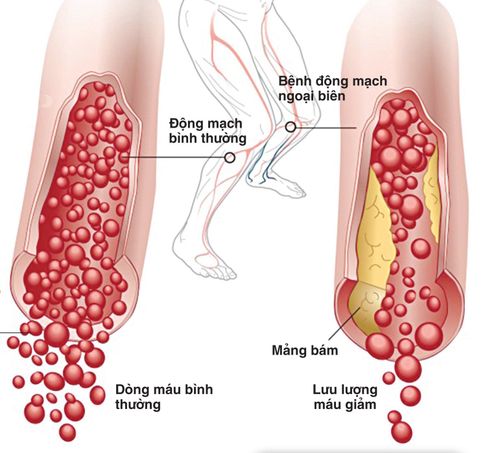
This is also a common symptom of systemic arteritis. Depending on the degree of vascular occlusion of the external carotid system, it will cause different visual effects.
Common symptom is that the patient will be afraid of light, especially bright light. Double vision or strabismus due to oculomotor paralysis. Transient blindness, white fog covering the eyes, visual hallucinations, visual disturbances...
Manifestations of visual disturbances caused by hormonal diseases often appear suddenly, develop rapidly and are irreversible. dress. It is possible to lose sight (due to paralysis of the optic nerve leading to permanent blindness) of the patient in just a few days, even a few hours if not detected and treated promptly.
2.3. Other symptoms
In addition to the above 2 typical symptoms, people with hormone disease also have some other symptoms as follows.
The temple area is slightly swollen, the skin surface is slightly red, it feels hotter to the touch than other skin areas. At the same time, you can see a thick, hard blood vessel, weak pulse or no pulse, if pressed, it will be very painful. Some patients may experience pain in both the tongue and throat. Difficulty swallowing or talking due to damage to the arteries that control activity in these areas.

Người mắc bệnh horton thường khó nuốt do tổn thương động mạch chi phối hoạt động vùng này
Patients often lose sleep due to persistent headaches and pain at night, loss of appetite, weight loss. Fever from mild to high fever. However, not all people with hormone disease experience all of these symptoms. Some patients have only persistent fever with no known cause. In some cases, there were additional symptoms of pseudo-polyarthritis, a lot of pain in the joints, especially the two sides of the shoulder joint, but there was no restriction on joint movement. This polyarthritis pseudo-symptom often precedes or accompanies the headache. In order to have an accurate conclusion that Horton's disease needs to be conducted some other tests such as erythrocyte sedimentation test, immune disorder, blood clotting disorder, especially selective temporal artery biopsy based on ultrasound doppler or perform an external carotid angiogram for the most accurate results.
3. Treating hormone disease as soon as possible brings good results
Experts and doctors have confirmed that the sooner the treatment of hormonal disease, the better the results will be for the patient. Corticosteroids such as prednisone, solu-medrol are considered the only effective treatment for hortoniasis. Once an accurate clinical diagnosis of this disease has been made, corticosteroid therapy should be started immediately to avoid adverse eye complications.
Nên sử dụng corticoid sớm để tránh các biến chứng xấu tới mắt
If the treatment step is highly effective, this is considered a real diagnostic test of hortonosis. With corticosteroid therapy, it is possible to save vision with only minimal damage.
Horton disease treatment results are often effective quickly, reducing fever and pain within the same day. Systemic arteritis also gradually subsided and the erythrocyte sedimentation rate returned to normal after only 1 to 2 months.
When using corticosteroids to treat hormone disease, it is necessary to use them daily according to the dose prescribed by the doctor, if used every other day or not regularly will not bring high efficiency. In the early stages of treatment, a combination of non-steroidal anti-inflammatory drugs (NSAIDs) can be used, and anticoagulants are also sometimes used to combat ischemia.
Vinmec International General Hospital with a system of modern facilities, medical equipment and a team of experts and doctors with many years of experience in medical examination and treatment, patients can rest assured to visit. examination and treatment at the Hospital.
To register for examination and treatment at Vinmec International General Hospital, you can contact Vinmec Health System nationwide, or register online HERE.
SEE MORE
Occlusion of the arteries: What you need to know Acute arterial occlusion of the extremities Learn about peripheral artery disease