This is an automatically translated article.
The article was consulted with Specialist Doctor I To Kim Sang - Internal Oncologist - Oncology Center - Vinmec Central Park International General Hospital.Worldwide, cervical cancer is the seventh most common cancer and the fourth most common cancer in women. In a year, more than half a million people are newly infected. This is a dangerous disease, accounting for a high rate in developing countries, where people have not been widely vaccinated against HPV as well as routine cervical cancer screening. So what is cervical cancer? Why is this disease dangerous? Let's find out together.
1. What is cervical cancer?
The cervix is the part of the female reproductive organs, connecting the vagina and the body of the uterus.Cervical cancer is a malignant disease of cells in the cervical region. The disease usually occurs in the transition zone between the squamous (squamous) epithelial cells of the outer neck and the glandular epithelial cells of the inner neck. Cancer is when cells grow, multiply, abnormally, uncontrollably, invade surrounding areas as well as metastasize to other parts of the body.
Women with cervical cancer are often at the age of sexual activity (30-45 years old), people under 20 years old rarely get the disease, while those over 65 years old find the disease often due to inadequate screening. good at the previous age.
2. Causes of cervical cancer
Most cases of cervical cancer are caused by infection with the human papillomavirus (HPV) in the high-risk group.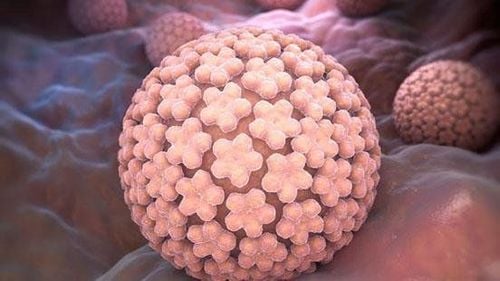
Human Papillomavirus (HPV) là nguyên nhân hàng đầu gây ung thư cổ tử cung.
Almost everyone of sexually active age gets HPV at least once in their life. However, not all HPV infections will lead to cervical cancer. When HPV enters the body, the body's immune system will be activated to fight the virus and most cases of HPV will be eliminated. HPV infection of any group is capable of self-resolving completely and leaving no sequelae. Approximately more than 90% of HPV is cleared spontaneously within the first year of infection and 70% occurs during the second year.
However, the body does not always defend successfully. A small percentage of HPV cases may persist in the basal cell layer of the cervix, especially in high-risk viral infections. It is prolonged HPV infection and chronic inflammation that cause precancerous lesions of the cervix (such as metaplasia in the order of mild, moderate, and severe). More than 50% of mild metaplasias are likely to regress on their own, 10% of moderate metaplasias are likely to get worse in 2-4 years, and about 50% of severe metaplasias will become cancerous in situ. cervix, but this ability is less common in young people.
Besides HPV, some other risk factors that can increase your chances of getting cervical cancer include:
Smoking: Women who smoke are twice as likely to get cervical cancer compared to women who smoke. with non-smoking women. Toxic substances in tobacco have been shown to cause many different types of cancer, including cervical cancer. Early sex, multiple sex, unprotected sex. Having multiple births (more than 5 children). Giving birth at a very young age (< 17 years old). Improper hygiene of the genital area. Chronic cervicitis. Immune system deficiency: In immunocompromised bodies, the risk of high-risk HPV infection increases, leading to an increased risk of cervical cancer. Using oral contraceptives for more than 5 years.
3. Signs of ectopic cancer
When experiencing one of the following signs of cervical cancer, you should see a specialist as soon as possible:
Ung thư cổ tử cung giai đoạn đầu không biểu hiện triệu chứng, khiến bệnh nhân chủ quan.
To meet the needs of women for gynecological cancer screening, Vinmec International Hospital currently offers a screening package and early detection of gynecological cancer, helping to detect 4 diseases early: Cancer cervical cancer, breast cancer, uterine cancer and ovarian cancer even if the patient has no symptoms.
Those who should use the Gynecological Cancer Screening and Early Detection Package include:
Female customers of screening age. Customers wishing to be able to screen for breast-gynecological cancers (cervical, uterine, ovarian). Customers with high risk of cancer - especially customers with a family history of breast and gynecological cancers. Women who are having symptoms of breast cancer, gynecology such as: Pain in the breast, lump in the breast, bleeding outside the menstrual period, abdominal pain ...
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.