This is an automatically translated article.
Lidocaine is widely known as a common anesthetic. In addition, it is also used in the treatment of dangerous acute arrhythmias. So what is Lidocaine and what should be noted during use?
1. What is Lidocaine?
Lidocaine has the active ingredient lidocaine, belongs to the group of anesthetics and antiarrhythmic drugs of group 1B. The content and dosage of Lodicaine is calculated according to the active ingredient lidocaine hydrochloride. Currently on the market there are many different dosage forms of Lidocaine with different concentrations:
Injectable form: 0.5% (50ml); 1% (2ml, 5ml, 10ml, 20ml, 30ml, 50ml); 1.5% (20ml); 2% (2ml, 5ml, 10ml, 20ml, 30ml, 50ml); 4% (5ml); 10% (3ml, 5ml, 10ml); 20% (10ml, 20ml); Solution for intravenous infusion in glucose 5%: 0.2% (500ml); 0.4% (250ml, 500ml, 1000ml); 0.8% (250ml, 500ml); 4% solution (25ml, 50ml), 5% solution (20ml) mixed with 5% glucose solution into 250-500-1000ml intravenous infusion of lidocaine hydrochloride 0.2%; 0.4%; 0.8%; first%; Drug form for external use in gel form: 2% (30ml); 2.5% (15ml); Ointment form: 2.5%; 5% (35g); Drugs for external use in solution form: 2% (15ml, 240ml); 4% (50ml); Cream: 2% (56g), 4% (5g, 15g, 30g). Mechanism of action of Lidocaine:
Lidocaine is essentially a local anesthetic of the amide group and has a medium duration of action. Lidocaine's mechanism of action is to block both the generation and transmission of nerve impulses through a reduction in the permeability of neuronal membranes to sodium ions. It can thus help stabilize membranes, inhibit depolarization, reduce propagation of action potentials, and ultimately block nerve impulse conduction; Lidocaine is widely used due to its advantages of faster, stronger and longer duration of action than procaine local anesthetics of the same concentration; Lidocaine is also indicated for the treatment of cases with a history of hypersensitivity/allergy to ester-type local anesthetics.

Lidocaine được bào chế ở nhiều dạng khác nhau
2. Indications and contraindications of Lidocaine
2.1. Indications Lidocaine is indicated in the following cases:
Lidocaine has a local anesthetic effect before conducting examinations, performing endoscopy, placing technical equipment in the body or conducting other procedures. ... purpose to relieve pain symptoms for patients; The drug lidocaine is used in sedation and nerve block anesthesia, including peripheral nerve block, sympathomimetic, epidural, sacral and spinal anesthesia; Treatment of certain acute ventricular arrhythmias after myocardial infarction or during cardiac engineering procedures (such as cardiac surgery or cardiac catheterization). Types of arrhythmias requiring treatment with lidocaine include: ventricular extrasystoles in myocardial infarction, ventricular tachycardia, and ventricular fibrillation. 2.2. Contraindications of Lidocaine Lidocaine is absolutely contraindicated in cases of allergy or hypersensitivity to local anesthetics of the amide group; People with Adams-Stokes, Wolff-Parkinson-White syndrome or some arrhythmias such as severe sinoatrial disorders, all-degree atrioventricular block, intraventricular block (without pacemaker); Severe heart failure; Porphyrin metabolism disorders.
3. Dosage and usage of Lidocaine
Dosage and usage in adults will depend on the purpose of treatment:
In case of using lidocaine for local anesthesia (sites such as mucous membranes of the nose, mouth, throat, trachea, esophagus, Tracheal, urinary - genitourinary tracts): Direct application of lidocaine hydrochloride solution (2 - 10%) with the maximum dose in a person weighing 70 kg is 500 mg. Note do not use repeat within 2 hours; Using lidocaine in layer-by-layer anesthesia: Injecting lidocaine hydrochloride directly into the tissue (concentration 0.5 - 1%). The dose of lidocaine depends on whether it is injected with adrenaline or not, if it is about 4.5 mg/kg, if not, the dose can be increased by 1⁄3 to 7 mg/kg; Lidocaine used in regional block anesthesia: Use by subcutaneous injection of lidocaine hydrochloride solution with the same concentration and dose as layer anesthesia; Nerve Blocking Anesthesia: Injection of lidocaine solution into the location near the nerve or into the peripheral nerve plexus will provide a broader anesthetic effect than the techniques mentioned above. To block nerves for 2 - 4 hours, the doctor may prescribe lidocaine (concentration 1 - 1.5%) with the same recommended dose as the above anesthetic methods; Acute treatment of ventricular arrhythmias: Loading dose of 3 - 4 mg/kg is given over 20 - 30 minutes, then can be maintained by continuous infusion at a dose of 1 - 4 mg/min. Dosage of lidocaine for other subjects: In patients with heart failure and liver disease, the total initial loading dose and maintenance infusion rate should be reduced. Initial dose 0.75 mg/min or 10 micrograms/kg/min; up to 1.5 mg/min or 20 micrograms/kg/min. Some patients with acute myocardial infarction may require higher than normal plasma lidocaine concentrations to maintain antiarrhythmic efficacy.
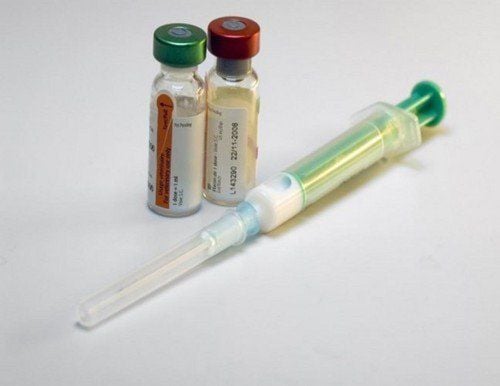
Lidocaine cần được sử dụng đúng liều lượng
4. Lidocaine side effects
Possible side effects of Lidocaine include:
Low blood pressure, headache when changing positions; So cold; Heart block, arrhythmia, can even cause heart failure and cardiac arrest; Shortness of breath, failure or cessation of breathing; Altered consciousness, coma, agitation; Slurred speech, convulsions; Anxiety disorder, feeling of euphoria or hallucinations; Itching, skin rash with swelling or numbness around the lips and tip of the tongue; Nausea, vomiting, paresthesia, visual disturbances such as blurred or double vision.
5. Some notes when using Lidocaine
5.1. General notes during drug use Do not use lidocaine preparations containing preservatives for the purpose of spinal, epidural or sacral anesthesia; Use with caution in cases of liver disease, heart failure, severe hypoxemia or respiratory failure, shock or conditions causing hypovolemia, incomplete heart block, bradycardia or atrial fibrillation. ; When used in severely debilitated or severely debilitated patients, caution should be exercised because of the possible risk of systemic toxicity with lidocaine; Do not inject anesthetics at sites of inflammation, infection, injury or burns because of the risk that the drug is absorbed more quickly, thereby causing systemic effects instead of local effects. 5.2. Signs of lidocaine overdose and management Symptoms of overdose include disturbances of consciousness (sedation, confusion, coma), onset of convulsions, respiratory arrest, cardiac toxicity (sinus arrest, blockade). atrioventricular, heart failure and hypotension), ECG arrhythmias (such as QRS and QT prolongation in severe overdose) with some systemic manifestations such as dizziness, paresthesias, chills, ataxia harmony and digestive disorders;
Treatment: Current treatment measures are mainly for the purpose of supporting common symptoms such as intravenous fluids, maintaining appropriate patient posture, controlling blood pressure, taking antiarrhythmic or antiarrhythmic drugs. convulsions). The use of sodium bicarbonate can assist in the recovery of prolonged QRS, bradyarrhythmias and decreased blood pressure. In some qualified cases, hemodialysis can be performed to speed up the elimination of lidocaine.
6. Lidocaine drug interactions
Drugs that are likely to interact with Lidocaine include:
Using Adrenalin in combination with Lidocaine may reduce the rate of absorption and reduce toxicity, so the duration of action of lidocaine may be longer; Amid anesthetics (such as bupivacaine, levobupivacaine, lidocaine, bupivacaine) used in combination with antiarrhythmic drugs lead to an increased risk of myocardial depression; Beta-blockers: Concomitant use may lead to decreased metabolism and increased risk of Lidocaine toxicity; Cimetidine inhibits the metabolism of lidocaine in the liver, leading to a higher risk of lidocaine toxicity when co-administered; Ranitidine may cause a slight decrease in lidocaine clearance; Succinylcholine used concomitantly with lidocaine may potentiate the effects of succinylcholine; Lidocaine has the potential to potentiate the effects of colchicine, tamoxifen, salmeterol or tolvaptan; The effect of Lidocaine will be higher when co-administered with Amiodarone, beta-blockers, conivaptan or decreased when used concomitantly with cyproterone, etravirin, peginterferon alfa-2b, tocilizumab; Concomitant use of Lidocaine with diuretics may lead to hypokalemia due to the antagonism of the 2 drug classes; The risk of ventricular arrhythmias or QT prolongation is higher when Lidocaine is co-administered with antipsychotics, prenylamine, adrenaline (intravenously) or 5HT3 antagonists (eg, Tropisetron, Dolasetron). Lidocaine is only effective when used correctly and in the right dose. Therefore, to safely take medicine, you need to follow your doctor's prescription. When the body occurs any symptoms after using the drug, it is necessary to immediately notify the doctor or go to the nearest medical facility for timely treatment.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.