This is an automatically translated article.
Pain has a "positive" physiological role by providing a warning of tissue damage, immobilizing the patient as well as the affected limb for faster recovery. However, pain causes a lot of adverse effects on the patient's recovery process, so what is the mechanism of pain perception and response?
1. What is pain receptors?
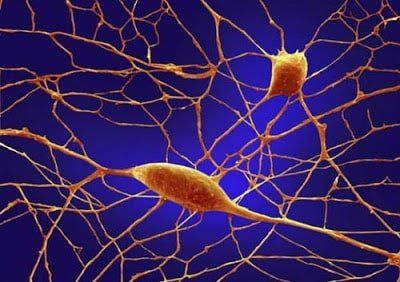
Pain receptors, also known as receptors, are a group of sensory neurons with specialized nerve endings widely distributed in the skin, deep tissues (including muscle) and joints) and most internal organs. They respond to tissue injury or potentially damaging stimuli by sending nerve signals to the spinal cord and brain to initiate pain perception. The receptor is equipped with specific molecular sensors, which detect too hot or too cold temperatures and certain harmful chemicals. Mechanoreceptors can also respond to stimuli that cause tissue damage, such as skin pinching or excessive muscle tension. Scientists are slowly unraveling the internal processes that lead to unpleasant pain.
Here is an example of what happens in pain.
You accidentally poked your finger into something sharp. This causes tissue damage, which is noted by the microscopic pain receptors in your skin. Each pain receptor forms one end of a nerve cell (neuron). It is connected to the other end of the spinal cord by a long nerve fiber or axon. When the pain receptor is activated, it sends an electrical signal up the nerve fiber. Nerve fibers are bundled with many other fibers to form peripheral nerves. The electrical signal travels through neurons inside the peripheral nerves to reach the spinal cord in the neck. In an area of the spinal cord called the dorsal horn, electrical signals are transmitted from neuron to neuron via junctions (synapses) by neurotransmitters. The signals are then transmitted from the spinal cord to the brain. In the brain, the signals travel to the thalamus. This is a sorting station that relays signals to different parts of the brain. Signals are sent to the tactile sensory cortex (responsible for physical sensations), the prefrontal cortex (in charge of thinking) and the limbic system (related to emotions).
Cơ quan thụ cảm là một nhóm các thế bào thần kinh cảm giác
2. How is the pain controlled?
There are many points on the pain signaling pathway that can intervene to control pain. One of them is the dorsal horn of the spinal cord. In this area, the "gate" mechanism can both let pain signals through or block it. This is the basis of the "gate" pain control theory described below.
The pain gate theory was put forward in 1965 by researchers Ronald Melzack and Patrick Wall. They suggested that there is a 'gate' mechanism in the central nervous system that opens to allow Pain signals pass through to reach the brain and close to block these signals.
When we feel pain, such as when we touch a hot stove, sensory receptors on the skin send a signal through nerve fibers to the spinal cord and brain stem, and then to the brain where the receptors are located. We feel pain, information is processed, and we perceive pain.
The gate theory suggests that when these pain signals enter the spinal cord and central nervous system (before they reach the brain), they can be amplified, attenuated, or even blocked. There are many accounts of how wounded people on the battlefield or in sports games did not feel the pain of their injuries until much later. This involves keeping the brain busy doing other things and closing the gate until it can pay attention to the signals.
Large diameter nerve fibers (A-beta fibers) responsible for transmitting tactile signals to the brain have the ability to close the pain gate and thus block signals from other smaller diameter nerve fibers that transmit sensation pain sensation. Another example is when a child falls and has knee pain - if he rubs his knee, the signal from that touch temporarily blocks the pain signal from traveling from the injured knee to the brain.

Não là nơi xử lý thông tin và khiến chúng ta cảm nhận được nỗi đau
3. Factors affecting pain perception
Severe pain quickly gets your attention and often produces a stronger physical response than mild pain. The location of the pain can also affect how you feel it. For example, pain coming from the head is harder to ignore than pain coming from other parts of the body.
The location of pain in the body does not always indicate where it is coming from. For example, the pain of a heart attack may be felt in the neck, jaw, arm, or abdomen. This is called projected pain and occurs because signals from different parts of the body often converge on the same nerve cells in the spinal cord.
Pain gate theory helps explain how the brain affects the way you perceive pain. Some of the following factors can affect how the body perceives pain:
Emotional and psychological state; Memories of past pain; Education; Expectations and attitudes towards pain; Beliefs and values; Age; Sex; and Social and Cultural Influence
4. Classification of pain
4.1. Nociceptive pain Nociceptive pain is pain caused by any injury to body tissues, such as a cut, burn, or fracture. Postoperative pain and cancer pain are other forms of nociceptive pain. This type of pain can be sharp, stinging, or throbbing. The pain may be constant or intermittent and may be worse with movement or coughing, depending on the origin of the pain.

Đau do cảm thụ thần kinh là đau bởi bất kỳ chấn thương nào đối với các mô cơ thể
4.2. Neuropathic pain is caused by an abnormality in the system that transmits and interprets pain - the problem could be in the nerves, spinal cord or brain. Neuropathic pain can be a burning, tingling, throbbing, or electrical sensation. One form of neuropathic pain is shingles pain, a skin disease caused by the varicella zoster virus. The virus causes neuritis, and this inflammation can cause ongoing pain, tingling, or burning sensations in some people, possibly for months after the shingles rash clears. People with neuropathic pain may feel pain from stimuli that would not normally cause pain, such as light touch or cold. They may also be more sensitive than usual to stimuli that are often painful. For example, when the affected area touches the bed sheet, the patient feels pain and can feel extreme pain even with the sting of the needle.
Neuropathic pain can be caused by many different processes.
Physical damage to nerves, causing abnormal signals. The spinal cord or brain does not successfully reduce the pain. 'Blow the wind'. When the spinal cord is constantly bombarded with pain messages coming from the C fibers, it amplifies the pain signals it sends to the brain. So you feel more intense pain. This is a short change, lasting only a few seconds or minutes, but it can set the stage for more lasting transformations. Increased efficiency in signal transmission at the junctions (synapses) between neurons. This is a complex process that can take many months. 4.3. Psychogenic pain This type of pain is psychologically caused or aggravated. Often the pain has a physical cause, but the degree of pain and reduced functioning is not commensurate with what most people with the same condition experience. This does not mean that the pain is not real, even if a physical cause cannot be found. Any kind of pain can be complicated by psychological factors. Doctors will also distinguish between acute and chronic pain.
+ Acute pain
This is a brief pain that warns the body is being hurt. This is a symptom of injury or disease at the tissue level and tends to resolve on its own like injury or illness.

Đau cấp tính là những cơn đau ngắn ngủi báo hiệu cơ thể đang bị tổn thương
+ Chronic pain
Chronic pain (also known as persistent pain) can be caused by ongoing tissue damage, such as osteoarthritis. However, in some cases, no physical cause is found for the pain or the pain persists long after the wound has healed. In many cases, chronic pain is itself a disease rather than a symptom of a disease process.
At the cellular level, several processes can cause pain to become chronic pain.
Pain receptors and neurons along pain pathways are excitable. Connections between neurons in the pathway can be altered. The brain and spinal cord fail to reduce pain signals. Pain receptors (usually in an inactive state) can be activated by inflammation. After a nerve injury, the nerve may regrow but not function properly. Chronic pain can persist for months or even years after the initial injury and can be difficult to treat. People with chronic pain may experience insomnia, anxiety, and depression, all of which can aggravate the problem. Chronic pain is an area of intensive research, with the hope of helping patients limit this pain in the future.
Any questions that need to be answered by a specialist doctor as well as customers wishing to be examined and treated at Vinmec International General Hospital, please register for an online examination on the Website for the best service.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: sciencedirect.com, mydr.com.au













