This is an automatically translated article.
Posted by Doctor Nguyen Van Phong - Heart Center - Vinmec Times City International General Hospital
Premature ventricular complexes (PVC) is an abnormal heart rhythm that originates in one of the two ventricles. Ventricular extrasystoles can occur in most people, including those without heart disease or those with existing heart disease, regardless of the severity of the heart disease.
1. Overview of ventricular extrasystoles
Ventricular extrasystoles may be more common in elderly patients, in patients with multiple comorbidities.
In patients without cardiovascular disease, the detection rate of ventricular ectopy is about 1% if a 12-lead ECG is recorded for 30-60 seconds and increases to 6% if a 2-minute ECG is recorded.
In adults, ventricular systole can be considered normal if it is less than 500 beats in 24 hours.
Ventricular extrasystoles can be classified in a variety of ways:
Patients with or without structural heart disease Clinical presentation: with or without symptoms Electrocardiographic morphology: right bundle branch block or left bundle branch block, unifocal or multifocal... Exercise related or not Frequency of occurrence Prognosis: potentially “malignant” e.g. ventricular extrasystoles in patients with structural heart disease, Idiopathic to early R/T ventricular extrasystoles. Idiopathic ventricular extrasystoles most commonly originate from the left ventricular outflow tract, the right ventricular outflow tract, or the aortic annulus
2. Clinical Manifestations
Most patients have no symptoms.
The most common symptom is palpitations or a feeling that the heart skips a beat
Patients may experience dizziness, a feeling of pulse in the neck or fatigue.
Ventricular extrasystoles rarely cause hemodynamic disturbances except in patients with severely reduced left ventricular function or ventricular extrasystoles occurring in patients with bradycardia.

Chóng mặt là triệu chứng thường thấy ở bệnh nhân ngoại tâm thu thất
3. Causes and risk factors and associated medical conditions
Cardiovascular disease:
Hypertension with left ventricular hypertrophy Acute myocardial infarction Heart failure Myocarditis Arrhythmogenic right ventricular cardiomyopathy Hypertrophic cardiomyopathy Congenital heart disease Tachycardia Idiopathic ventricular tachycardia A number of other conditions not related to cardiovascular disease:
Chronic obstructive pulmonary disease (COPD) Sleep apnea syndrome Pulmonary hypertension Endocrine disease (thyroid, glandular) Adrenal or gonadal abnormalities) may be associated with ventricular extrasystoles. Use of stimulants and drugs: nicotine, alcohol, caffeine, sympathomimetics (beta-agonists, vasopressors stuffy nose, antihistamines) or some opiates: cocaine, amphetamines
Suy tim có thể là nguyên nhân gây ngoại tâm thu thất
4. Complications
Most cases of ventricular extrasystoles are asymptomatic and have no dangerous complications. However, some cases of ventricular extrasystoles can be a trigger for other complex and dangerous arrhythmias.
Rarely if ventricular extrasystoles occur in a patient with underlying heart disease that can lead to dangerous arrhythmias that can even cause
5. Tests and diagnostics
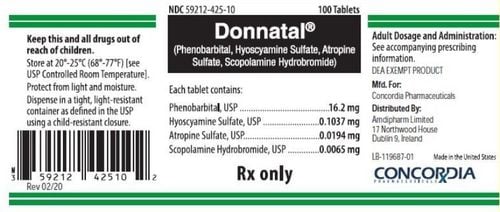
Electrocardiogram ECG :
If your doctor suspects you have ventricular extrasystoles, you will be ordered to do an electrocardiogram (ECG).
ECG can detect ventricular extrasystoles, extrasystoles, origin or detect underlying heart disease (coronary artery disease...)
If ECG fails to detect ventricular extrasystoles, physician may have you wear a 24-hour ECG monitor (Holter ECG).
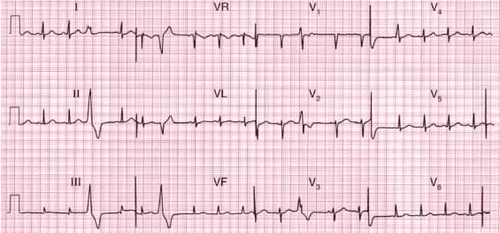
Hình 1: Ngoại tâm thu thất
Stress testing :
In some cases, your doctor may order you to perform a stress test. You will have continuous electrocardiogram monitoring during exercise (on a treadmill or bicycle).
Stress testing can determine the severity of ventricular premature beats: If ventricular premature beats decrease or disappear with exercise, it is usually safe and functional. Conversely, a higher frequency of ventricular premature beats may predict future dangerous arrhythmias. In addition, stress testing can help detect underlying coronary artery disease.

Hình 2: Gắng sức bằng thảm lăn

Hình 3: Gắng sức bằng xe đạp lực kế
Cardiovascular imaging:
All patients are assigned to do echocardiography to evaluate the structure and function of the heart
In some cases, if in doubt, the doctor may order you to perform the following tests: more advanced imaging studies such as coronary angiography or cardiac magnetic resonance
Blood tests:
There is no specific test for extrasystoles. However, your doctor may order the following tests depending on your history and physical examination:
Electrolytes, especially potassium and magnesium Blood count Thyroid hormone BNP or Pro BNP Arterial blood gases ( COPD or other chronic lung disease) Digoxin levels (if patient is taking Digoxin)
6. Treatments and Medicines
The decision to treat ventricular extrasystoles depends on the clinical status of the patient (symptomatic or asymptomatic), the presence of concomitant structural heart disease or not.
In cases where the trigger is related to stimulant use, lifestyle changes play an important role (For example, reducing or quitting alcohol, coffee, tea, stopping drug use. ..)
Patients with no symptoms, no structural heart disease usually do not need treatment.
Patients with no symptoms but with reduced left ventricular function are often prescribed beta-blockers at low doses.
Most patients with symptomatic ventricular extrasystoles usually receive treatment to clear or reduce symptoms. Before initiating treatment, it is necessary to identify and correct the triggering factors (use of stimulants, drugs, thyroid disease or electrolyte disturbances).
For most symptomatic patients, the first-line recommendation is a beta-blocker (or to a lesser extent a non-dihydropyridine calcium channel blocker) or other antiarrhythmic or ablation therapy. by radio waves (RF).
In case of failure of medical treatment, the patient can be advised to perform electrophysiological exploration and RF treatment.
The Cardiology Clinic under the Vinmec International General Hospital system nationwide is a reliable address with full modern equipment and a team of experienced doctors who will help you make the right decisions. most, exclude dangerous causes, advise you on the appropriate monitoring and treatment direction.
To register for examination and treatment at Vinmec International General Hospital, you can contact the nationwide Vinmec Health System Hotline, or register online HERE.