This is an automatically translated article.
The article was written by MSc Vu Duy Dung - Doctor of Neurology, Department of General Internal Medicine - Vinmec Times City International Hospital.Primary infection with VZV causes chickenpox in children, a common illness before vaccines became widely available since 1995. Humans are the only source of the highly contagious airborne virus. In this regard, the incidence of chickenpox has decreased following the availability of a vaccine.
Vaccines prevent about 90% of cases, but some people who have been vaccinated may still have mild symptoms of the disease. Manifestations of latent VZV infection are common in neurological clinical practice. VZV can affect all sites on the nerve axis and has practically caused disease in the brain parenchyma, spinal cord, subarachnoid space, arteries, eyes, and skin.
1. Shingles, Postherpetic neuralgia, and Shingles without blisters
VZV can persist in the dorsal root ganglia after primary chickenpox, possibly by migrating into the dorsal root ganglia from the skin via sensory nerves or by hematogenous dissemination.
The virus may reactivate intermittently in the dorsal root ganglia, but the immune system will usually suppress it before it causes clinical symptoms. As the virus reactivates and travels along a sensory nerve to the skin, it infects the epithelial cells and the vesicular lesions of the shingles become evidently distributed in a segment of the skin, with All vesicles are at the same stage of development.
Inflammation of the nerves and skin causes severe pain (called shingles, shingles, or acute herpes neuralgia) and can cause permanent nerve damage, known as semiherpetic neuralgia acute if pain persists for more than 30 days or postherpetic neuralgia if pain persists for more than 4 months after the appearance of vesicles.
No obvious vesicles but the patient reports shingles on the skin segment, it could be reactivated VZV in the dorsal root ganglia and the patient has zoster sine herpete, may respond to antiviral therapy.
The concept of vesicular pain has been recognized as causing a painful polyneuritis and has been expanded to include essentially all manifestations of VZV without visible vesicles can see.

2. Cerebellitis, Encephalitis, Myelitis, and Meningitis
VZV can cause central nervous system dysfunction, most commonly cerebellitis, in about 1 in 4000 cases of chickenpox, with neurological signs and symptoms that may include ataxia, nystagmus vomiting, headache, stiff neck, and lethargy. Neurological manifestations may present weeks before to several weeks after vesicle onset, and patients may also present with meningeal irritation and fever.
Other CNS signs and symptoms, such as hemiparesis, sensory abnormalities, tone abnormalities, tendon reflex abnormalities, or seizures, suggest a more diffuse encephalitis. Acute and subacute delirium are common in VZV encephalitis, and mortality can be as high as 10% to 25%.
Chronic VZV encephalitis has been seen in immunocompromised patients, such as those with acquired immunodeficiency syndrome (AIDS), and may also be associated with multifocal leukoencephalitis, encephalitis ventricles, and myelitis in such patients. Typical symptoms and signs of myelitis include lower extremity weakness, circular muscle disturbances, and upper motor neuron signs.
If meningeal irritation is present in the absence of other symptoms of CNS dysfunction, clinicians should consider VZV as a possible cause of meningitis.
3. Shingles of the eyes, Shingles of the ears, Cranial neuropathy, and radiculitis
When VZV reactivates according to the V1 branch of the trigeminal nerve, the term used as ophthalmic shingles, patients often have periorbital vesicles including the base of the nose (Hutchinson's sign).
Ocular shingles is a manifestation of VZV of particular concern, as it can lead to a variety of ocular complications, including partial or complete cranial nerve disease of the III, IV, or cranial nerves. BECAUSE; acute or progressive retinal necrosis; retinal detachment ; keratitis ; uveitis ; iritis ; and scleritis/episcleritis.
Furthermore, the development of contralateral hemiplegia due to ischemic stroke or hemorrhagic stroke or the occurrence of myocardial infarction may occur weeks to months after the onset of shingles in the shingles. eye.

Zona distribution in the ear, short called ear shingles or Ramsay Hunt syndrome, is related to VZV reactivation in the knee ganglia of the facial nerve. Manifestations include blisters on the outer ear, ipsilateral half of the tongue, or the roof of the mouth; peripheral cranial nerve VII with facial weakness and possibly loss of taste in the anterior two-thirds of the tongue; and possibly VII I cranial nerve dysfunction with hearing loss and vestibular symptoms.
Cranial nerve diseases can also be seen in shingles in C2 or C3 skin segments, whereas radiculitis and peripheral neuropathy leading to segmental motor weakness can be seen in shingles distributed in the neck, chest or the same belt.
4. Vascular disease and stroke
Ischemic stroke, hemorrhagic stroke, and myocardial infarction are associated with prior VZV infection, especially ophthalmic shingles, and the risk of a vascular event following VZV infection is increased in at least 1 year after infection. VZV has been implicated as a contributing factor in 30% to 40% of ischemic strokes and transient cerebral artery disease in children.
In general, transient ischemic attack, stroke, or VZV-associated CNS vasculitis can be suspected when a patient has a recent presentation of VZV infection, when neuroimaging Menstrual stroke with ischemic stroke (more often ischemic than hemorrhagic) in deep structures or at the gray-white matter border and may increase contrast enhancement, when CSF tests show mononucleosis (usually less than 100 cells/mm3) which may be associated with an increased red blood cell count, or when angiography confirms localized stenosis of the artery or a granular artery (in large or small arteries [or both] are common).
Other manifestations of VZV vascular disease include spinal infarction, intracerebral or subarachnoid hemorrhage, cerebral aneurysm, dissection, vasodilation, and increased vascular enhancement on pulsed MRI T1 after injection of contrast agent from .
Some experts have considered VZV vascular disease as a possible mechanism for progression to encephalitis, cranial neuropathy, peripheral artery disease, cerebral venous sinus thrombosis, and giant cell arteritis granulomatous granuloma of the aorta or temporal artery.

5. Diagnosis
The diagnosis of chickenpox, usually in a child with no history of illness who presents with mild systemic symptoms and diffuse vesicles, can be clinical; Similarly, vesicular segmentation of the skin of Zona allows the clinical diagnosis in the majority of cases.
Since there is no asymptomatic shedding of VZV virus (as opposed to HSV or CMV), detection of VZV virions, antigens or nucleic acids is diagnostic of an active viral infection. VZV can also be cultured using diploid human embryonic kidney or lung cells; however, the virus is unsustainable and has a low cultability rate, low sensitivity, and high cost.
A more pragmatic approach to determining the presence of VZV may include direct immunofluorescence staining using monoclonal antibodies, PCR for detection of VZV nucleic acids (which can also distinguish wild-type VZV from vaccine-associated VZV), and detect VZV IgG in CSF.
In patients presenting few signs and symptoms, the diagnosis of VZV-associated disease depends on a high index of suspicion; a complete history of previous exposure to VZV and any manifestations of viral infection; and serological, pathological, or imaging tests confirm VZV infection.
In cases of cerebrovascular disease, CSF PCR of VZV DNA is only 30% sensitive (possibly because of the delay of several weeks from the onset of active VZV infection to the onset of CNS symptoms). Diagnostic sensitivity is increased to 93% with the addition of IgG VZV in CSF, and additional testing of IgM VZV in CSF can also improve diagnostic sensitivity.
The VZV CSF antibody index can be calculated to determine if the intramedullary biosynthesis of VZV-specific IgG is increased by the formula below:
VZV antibody index CSF = IgG VZV CSF ÷ IgG VZV blood barTotal CSF IgG or albumin ÷ total serum IgG or albumin
The CSF antibody index is considered elevated when the value is 1.5 or higher and is used to avoid the possibility of false-positive detection of anti-VZV IgG antibodies in CSF because of serum infection.
6. Treatment

Chickenpox is generally a self-limiting infection in otherwise healthy children, and no specific treatment is recommended, but aspirin should be avoided because of its association with Reye's syndrome.
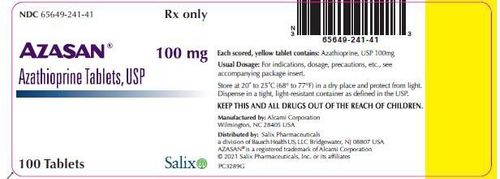
In adults, if there is clinical concern about the possibility of VZV infection progressing or VZV reactivation, treatment with antiviral agents is recommended. Antiviral drugs shorten the duration of the rash and help cure shingles more quickly but are not required in immunocompetent young patients under 50 years of age.
For shingles in patients over 50 years of age, immunocompromised patients, or patients with shingles ophthalmic or shingles, systemic antiviral therapy for 7 to 10 days is recommended.
In patients with CNS manifestations of VZV, including vascular disease, or who have non-vesicular shingles or diffuse VZV, intravenous acyclovir is recommended for 14 days.
A short course of oral prednisone (1 g/kg) is advocated by some experts for the treatment of shingles, shingles, and VZV vascular disease. Symptomatic treatment of acute, subacute, and postherpetic neuralgia can be achieved with the use of topical analgesics (eg, lidocaine patch, trolamine salicylate, aloe vera [aloe vera] or capsaicin), anticonvulsants (eg, gabapentin, pregabalin, oxcarbazepine, divalproex sodium, levetiracetam), tricyclic antidepressants (eg, amitriptyline, nortriptyline), local anesthetic injections to selectively block sympathetic nerves epidural nerve block or cold, or, in carefully selected and refractory cases, opioid analgesia (eg, tramadol, controlled release oxycodone, controlled release morphine, or methadone) .
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Articles source references:
Baldwin KJ, Cummings CL. Herpesvirus Infections of the Nervous System. Continuum (Minneap Minn) 2018;24(5, Neuroinfectious Disease):1349-1369.