Dao Duc Dung*, Le Hai Binh, Chu Anh Kiet, Vo Thanh Viet Anh, Dinh Thuy Duong, Pham Duc Huan #
* First author
# Corresponding author
1.Background:
The definition of value in health care was first introduced in the book Redefining Health Care: Creating Value-Based Competition on Results as the measured improvement in a patient’s health outcomes for the cost of achieving that improvement. A healthcare that is value-based should provide cost-effective ways to improve patient health outcomes by optimizing its available resources. This concept, however, is entirely novel in Vietnam as the prevailing norm in the country remains to be the traditional fee-for-service model.
Esophageal cancer is difficult to treat and often ends up with poor outcomes. According to GLOBOCAN, in 2020, there was approximately 3281 new cases and 3080 deaths in Vietnam. Esophageal cancer requires multimodal treatment in which esophagectomy is considered as the cornerstone, however, it is a highly invasive procedure with several serious postoperative complications that may result in poor quality of life, extended hospital stay, and even mortality. Moreover, esophagectomy itself is a complex procedure that only a limited number of facilities are able to perform. Due to those reasons, overall costs of surgical hospitalization episode is elevated and makes it difficult for patients to access to the treatment they need. To improve esophageal cancer patient experience is an urgent task, however, it can be a tremendous challenge to overcome.
Taking challenges as opportunities, Vinmec Times City Hospital established Esophageal Cancer Integrated Practice Unit (IPU) – a multidisciplinary team with participation of departments providing treatment and care for esophageal cancer patients. By standardizing care pathway and practice, applying ERAS (Enhanced recovery after surgery) protocols, providing staff training, eliminating wastes in esophageal cancer patient care process, evaluating patient-reported outcome measures (PROM) as well as fostering continuous quality improvement initiatives, the Program has made progress in improving esophageal cancer patient experience through a value-based approach.
2.Goals:
Pursuing comprehensive care and excellent clinical outcomes while optimizing costs is a challenging goal. In order to conquer this mission, the Program was applied in 19 esophageal cancer patients admitted from Quarter 2 2022 to Quarter 4 2023 with the following objectives:
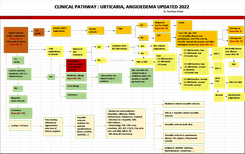
- To improve and maintain Clinical Pathway (CP) compliance rate at the highest level (95-100%).
- To apply ERAS protocols for 100% of patients who undergo esophagectomy. The ERAS protocols are multimodal perioperative care pathways designed to achieve early recovery after surgical procedures. The protocols include pre-operative counselling, optimization of nutrition, standardized analgesic and anesthetic regimens, and early mobilization.
- To shorten Intensive Care (ICU) length of stay (LOS) and post-operative hospital LOS.
- To reduce surgical procedure-related complications (including any major complications noted during the operation and/or within 30 days after the operation).
- To accelerate recovery process of patients after esophagectomy.
- To improve patient-reported outcome measures (PROM). PROM are reports of health status that come directly from the patients, reflect quality of the treatment and care process. In this Program, EORTC QLQ-OES18 questionnaire was utilized as esophageal cancer-specific PROM.
- To optimize total costs of the surgical hospitalization episode by at least 10%.
3.Activities:
Phase 1 – Preparation (Quarter 1 2022): In Quarter 1, the hospital leadership launched Esophageal Cancer IPU Program in a kick-off meeting with leaders of departments providing treatment and care to esophageal cancer patients. IPU Medical Director and its members were appointed. The IPU team developed backbone documents including CP, a compliance checklist (to assess effectiveness of training, monitor and ensure the CP is followed seamlessly and uniformly, thereby reducing unnecessary orders that may elevate financial burden), patient education materials and a list of indicators for measurement. Staff training was organized. Data of the past were collected to determine the baseline and areas for improvement.
Phase 2 – Implementation (Quarter 2 – 3 2022): IPU periodic meetings were hold on a quarterly basis. Based on historical data, esophageal cancer surgery and its related matters including compliance with CP, pain management and analgesia, antibiotic days, nutrition, post-operative length of stay, recovery process, quality of life and patient-reported outcomes were selected as the priority areas for improvement. The ERAS (Enhanced recovery after surgery) protocols were adopted and implemented from Quarter 2 2022. From Quarter 4 2022, EORTC QLQ-OES18 questionnaire (PROMs) was administered to all esophageal cancer patients before surgery, at 1 month and at 3 months after surgery to collect PROs.
Phase 3 – Optimization and maintenance of the value-based model (Quarter 4 2022 – now): In order to maintain and further improve clinical outcomes and optimize costs, every quarter, the team determined one area of esophageal cancer treatment and care process for improvement and implemented a quality improvement (QI) project targeting at the area accordingly. The IPU model and value-based approach were adopted for management of other types of cancers within Vinmec Times City Hospital and member hospitals in Vinmec Healthcare System.
4.Results:
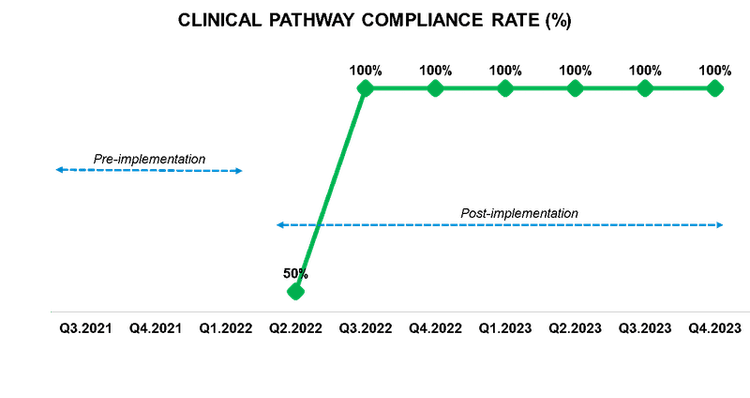
CP compliance rate:
Compliance rate increased from 50% in Quarter 2 2022 to 100% and was sustained in the subsequent quarters.
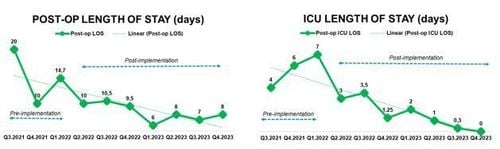
Clinical outcomes:
A steady decline has been observed in both post-operative LOS and ICU LOS since the implementation of ERAS protocols. At baseline, the post-operative LOS was averagely 14.9 days. By the end of 2023, the average post-op LOS had reduced to 7-8 days, which was significantly shorter than the durations observed in other domestic and foreign facilities. The ICU LOS at baseline was averagely 5.8 days, and the protocols further reduced it to 0 – 0.3 day after 6 quarters of implementation.
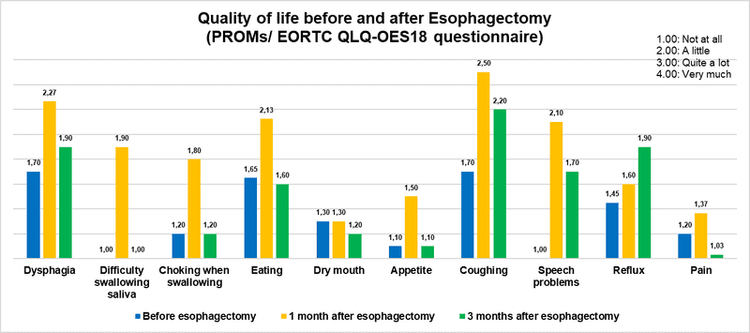
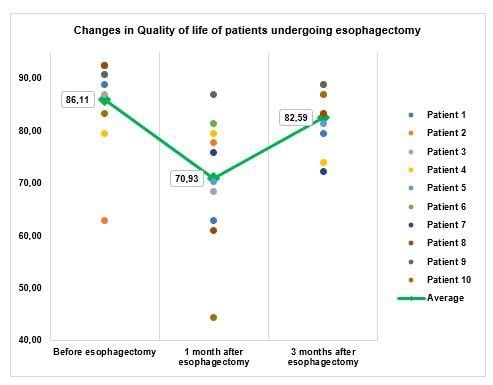
PROMs:
The PROMs surveyed ten esophagectomy-related problems. Overall, the post-esophagectomy patients experienced an average of 15.18 % decline in quality of life at one month, followed by recovery at three months (about 3.52% lower than their status before surgery). Notably, at the three-month mark, all of the patients reported complete alleviation of difficulty swallowing saliva and nine out of ten surveyed patients no longer suffered from pain including stomach pain, chest pain, and pain during meals. The only concern that exhibited deterioration at three months was reflux. Thus, patient and family education regarding nutrition and diet will be the priority and the team expects that in upcoming quarters, this intervention will help elevate overall status at 3 months to the level that is equal to or greater than that before surgery.
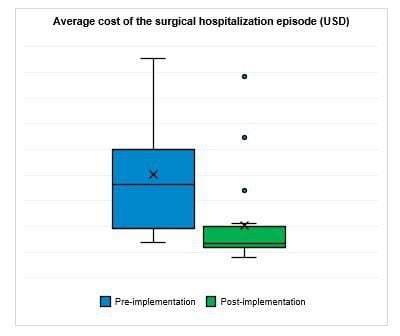
Cost optimization:
Following the implementation of ERAS and series of interventions aiming at standardizing care pathway and practice, enhancing recovery process, and reducing antibiotic days, the average cost of the surgical hospitalization episodes in Phase 2 and 3 decreased by approximately 22.08% compared to the previous period.
5.Closing argument:
The Program has shown positive results in both clinical outcomes and cost optimization. Due to the standardization of clinical practice and the application of ERAS protocols, our esophageal cancer patients could benefit faster recovery process, shorter length of stay without any major complications that may extent their hospital stays or cause readmission. PROMs monitoring followed with corresponding interventions has contributed to improvement of post-esophagectomy patients’ quality of life. Beside positive changes in the clinical outcomes, the overall costs of the surgical hospitalization episodes were also optimized thus increased more values to the patients.
Moreover, the Program has successfully engaged continuous improvement culture among personnel of departments involved in the process. It has laid a solid foundation for future expansion of the IPU model for other types of cancers in Vinmec Times City Hospital as well as member hospitals in Vinmec Healthcare System.
With the promising results, the Esophageal Cancer Program has demonstrated efforts of Vinmec Healthcare System in introducing value-based approach in Vietnam. Vinmec Healthcare System, as the only private and not-for-profit healthcare organization in the nation, will have the chance to catalyze for the shift of volume-based to value-based model in the healthcare landscape in Vietnam.
REFERENCES:
Porter ME, Teisberg EO. Redefining Health Care: Creating Value-Based Competition on Results. 2006Boston, MA: Harvard Business School Press.
https://www.nuhs.edu.sg/About-NUHS/nuhs-value-based-healthcare/Pages/default.aspx
https://gco.iarc.fr/today/data/factsheets/populations/704-viet-nam-fact-sheets.pdf
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3202008/
https://tapchiyhocvietnam.vn/index.php/vmj/article/view/496/380
https://tapchi.ctump.edu.vn/index.php/ctump/article/view/384/372
https://repository.kulib.kyoto-u.ac.jp/dspace/bitstream/2433/154600/1/s00464-011-1883-y.pdf
https://www.annalsthoracicsurgery.org/article/S0003-4975(01)03584-6/fulltext