This is an automatically translated article.
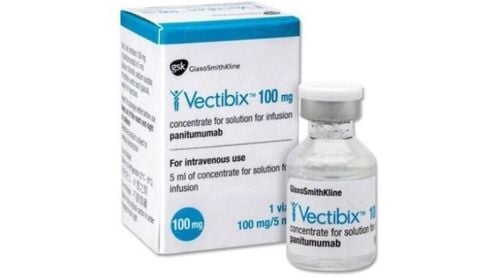
Cetuximab is a monoclonal antibody that binds to specific targets on cancer cells, thereby stimulating the immune system to destroy them. This is one of the modern cancer treatments. So, what does Cetuximab do and in what cases is it indicated?
1. What does Cetuximab do?
Monoclonal antibodies are created in the laboratory with the aim of binding to specific targets on different types of cancer cells. This antibody then stimulates the immune system to attack the cell it attaches to, resulting in the immune system killing the cell.
Cetuximab is a man-made version of a natural human antibody and inhibits the epidermal growth factor receptor (EGFR). EGFR is an abnormally overexpressed protein in many cancers, and inhibition of EGFR leads to a reduction in malignant cell growth as well as a decrease in the production of other factors that contribute to cancer metastasis. Cetuximab is indicated for the treatment of head, neck and colorectal cancer. In which colorectal cancer needs to test positive for the KRAS mutation, the patient should be tested for this mutation before starting Cetuximab.
2. Indications and contraindications of the drug Cetuximab
Cetuximab is indicated in the treatment of patients with non-mutant RAS metastatic colorectal cancer with expression of epidermal growth factor receptor (EGFR):
In combination with irinotecan-based chemotherapy ; As first-line drug when combined with FOLFOX (Irinotecan, Fluorouracil, Leucovorin); Monotherapy in patients who have failed Oxaliplatin and Irinotecan-based therapy or who are intolerant to Irinotecan. Cetuximab is also used in the treatment of squamous cell cancers of the head and neck:
In combination with radiation therapy when the disease is locally advanced; In combination with platinum-containing chemotherapy regimens when the disease recurs and/or metastasizes. Cetuximab is contraindicated in patients with severe hypersensitivity reactions (grade 3 or 4) or when cetuximab is combined with axaliplatin-containing chemotherapy in patients with RAS-mutated colorectal cancer (mCRC) or without clear RAS mCRC status.
3. How to use Cetuximab?
Cetuximab is manufactured for intravenous administration at a dose according to the patient's weight. The frequency of Cetuximab infusion depends on the type of cancer and other treatments the patient is receiving. Before taking the first dose of Cetuximab, the patient will be prescribed certain medications such as Diphenhydramine to prevent an infusion reaction.
The recommended infusion time of Cetuximab is 120 minutes. For weekly doses, the recommended infusion time is 60 minutes. The infusion rate should not exceed 10 mg/min. The first dose of Cetuximab should be infused slowly and the infusion rate should not exceed 5 mg/min.
4. Side effects of the drug Cetuximab
4.1. Infusion reactions Some patients will develop a reaction to Cetuximab, especially at high risk at the first dose. Reactions may include chills, fever, shortness of breath, shortness of breath, hoarseness, itching, or low blood pressure. Patients should notify their healthcare provider immediately if they experience any of these symptoms. Most patients will be given some medication to prevent this reaction by their doctor and continue to be monitored for at least 1 hour after the Cetuximab infusion is completed.
4.2. Heart problems Cetuximab can cause heart problems, including cardiac arrest and heart attack. Patients with a history of coronary artery disease and/or radiation therapy are the highest risk group. Patients should notify their doctor or go to the emergency room immediately if they develop chest pain, have trouble breathing, or feel dizzy or faint.
4.3. Electrolyte disturbances Cetuximab may affect normal levels of electrolytes, including magnesium, calcium and potassium. This can even happen after the patient has completed treatment. Your doctor will monitor your electrolyte levels during and for at least 8 weeks after completing treatment with Cetuximab.
4.4. Nail and skin changes Cetuximab can cause nail and skin related side effects. Patients may develop a rash that, although it may resemble acne, is not and should not be treated with acne medications. A skin rash may be accompanied by redness, swelling, scaling, and dryness, and is painful for the patient. The rash may be worst during the first few weeks of treatment but may continue until treatment with Cetuximab is stopped.
Some measures to manage the skin of patients taking Cetuximab include:
Use alcohol-free lotion or emollient cream at least 2 times a day, including after bathing; Sun exposure can worsen the rash, so people should use sunscreen with an SPF of 30 or higher and wear a hat and sunglasses to protect their head and face; Shower with cool or warm water; Use soaps, perfumes and laundry detergents that do not contain alcohol or dyes; Wear gloves when doing housework or gardening; Drink plenty of water and try not to scratch or rub your skin. During treatment with Cetuximab, patients may develop dermatitis around the nail bed with redness, swelling, or pus. This condition can cause the nail to grow "hedges" or fall off. This side effect of Cetuximab may appear several months after starting treatment but may persist for many months after stopping treatment.
4.5. Increased sun sensitivity Cetuximab may make a patient's skin more sensitive to the sun, which could lead to severe sunburn or a rash. Sensitivity to the sun may persist even after treatment ends. Limit sun exposure while taking Cetuximab and for at least 2 months after the last dose.
Some measures to protect the skin while taking Cetuximab:
Avoid the sun between 10 am and 2 pm; Apply sunscreen (at least SPF 15) daily; Wear sunglasses, hats and long clothes; Find shade whenever possible. 4.6. Nausea, vomiting Talk to your treating doctor to find medications that work for this side effect. In addition, patients can change their diet and limit things that aggravate nausea and vomiting, such as limiting overeating, saying no to fatty, high-fat foods. taste or acidic (such as lemon, tomato, orange).
4.7. Muscle or Joint pain and weakness Your doctor may recommend medications and other strategies to help relieve pain caused by Cetuximab.
4.7. Some less common side effects of Cetuximab Hair changes: While taking Cetuximab, a patient's eyelashes may grow very fast, very long and cause discomfort to the eyes. Patients should talk to their doctor about how to best manage this side effect. In addition, the patient's hair may become frizzy, thin, or brittle. However, these changes tended to disappear after treatment with Cetuximab was discontinued; Lung problems: Cetuximab can cause interstitial lung disease (ILD), especially in people who already have lung problems. Patients can have breathing tests (pulmonary function tests) performed periodically and call their doctor at once if they have trouble breathing, cough, wheezing, or have rapid breathing.
5. Fertility effects of Cetuximab
If the fetus is exposed to Cetuximab, it can lead to birth defects, so the patient should not become pregnant or father a child during treatment with this medicine. If the patient becomes pregnant, the doctor will review and decide whether the patient should take Cetuximab or not. Practicing effective forms of birth control is essential during treatment and for at least 6 months after stopping treatment with Cetuximab. Even if the menstrual cycle has ceased in women or there is evidence of a lack of sperm production in men, conception and pregnancy can still occur.
Patients taking Cetuximab should not breastfeed until at least 2 months after the last dose.
Above is the information about the drug Cetuximab. Patients should carefully read the information on the instructions for use before use.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.