This is an automatically translated article.
Post by Master, Doctor Mai Vien Phuong - Head of Department of Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital
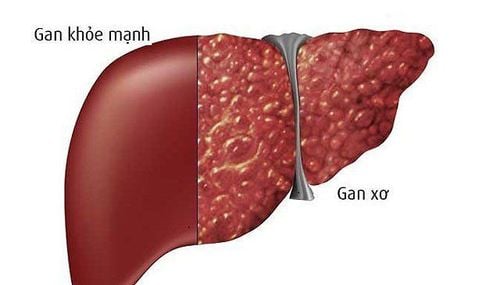
Liver hemangioma is evaluated as a benign tumor, formed by clusters of blood vessels. According to the assessment, the disease often has no clinical manifestations, so the detection and treatment of liver hemangiomas are often through the patient's examination for other diseases.
1. Overview of treatment of liver hemangiomas
Due to its rarity, the diagnosis of liver hemangiomas on imaging (and even histology) is difficult. Therefore, the clinical management of patients with hepatic hemangiomas should be performed in specialist centers for multidisciplinary work involving radiologists, pathologists, and hepatologists. Performing a liver biopsy is recommended to better balance the risks of surgery (eg, removal of a central tumor carries a higher risk than the risk of tumor-related complications. In the case of asymptomatic liver hemangiomas, with no cytologic loss on biopsy, but at high risk of complicated resection, routine imaging is preferred. found that the majority of patients were treated with surgical resection (84% and 76% of patients in two large case series).For other patients, frequent imaging follow-up was justified by the There is uncertainty surrounding the risk of liver hemangioma progression Although the risk of tumor recurrence after resection or metastasis has rarely been described, determining factors by imaging and especially histology predicting an unfavorable course is essential for a collective treatment decision.Moreover, patient compliance with regular imaging will also is an important argument in decision making.
2. Imaging follow-up time for liver hemangiomas
The optimal imaging follow-up period is not well established, but the first imaging assessment may take place after one year, as the liver hemangioma has been described as increasing only 0.77 cm per year for one year. A series of 29 patients underwent radiological follow-up, and radiographic progression was affected only in 6 out of 29 patients (20%). Thereafter, imaging surveillance may be performed twice a year, but the frequency will depend on the extent of tumor progression during the early years of follow-up. Obviously, persistent tumor progression on consecutive imaging would require surgical approach. Therefore, surgical resection is recommended when there is uncertainty about the histological nature of the lesion after liver biopsy, tumor progression on imaging, tumor-related symptoms, and when the tumor is exceed 5 cm. The recurrence rate after surgical resection was 2.4% (6 out of 246 patients in the series reported by Klompenhouwer et al.). The rate of local or distant recurrence after resection is 10% in cases of hemangiomas of the epithelial type.3. The role of liver transplantation
Liver transplantation (LT) is sometimes erroneously performed to diagnose suspected cholangiocarcinoma or hemangioma mimicking hepatocellular carcinoma. These misdiagnosis further emphasize the interest of systemic liver biopsy as well as the expertise in imaging and pathology. Since the first liver hemangioma liver transplant was reported in 2010, other exceptions have been added to liver transplantation performed as a last resort for unresectable liver hemangiomas. removed due to excessive size or a significant number of liver tumors.
4. Other Alternative Treatment Options
Other alternative treatment options have been reported, such as radiofrequency ablation, arterial embolization or the use of sirolimus. mTOR inhibitors, including sirolimus and everolimus, are immunosuppressive molecules used in transplantation and also have antiproliferative properties. In a multicenter, double-blind, placebo-controlled, phase 3 trial (EXIST-2), 118 patients had at least one renal angiomyolipoma greater than 3 cm associated with the diagnosis of tuberous sclerosis complex. or sporadic LAM were randomized to receive everolimus 10 mg orally/d (n=79, mean dose: 8.6 mg/day, median duration: 38 weeks) or placebo (n=39 ). The trial showed a beneficial effect of everolimus in reducing the size of Angiomyolipoma (response rate: 42% vs 0% in the placebo group; P < 0.0001). Response assessed as composite endpoint consisted of ≥50% decrease in Angiomyolipoma volume.5. What do the studies say?
The favorable results reported in the EXIST-2 trial led to an open label extension by the same author. This study demonstrated a clear benefit of everolimus for patients who continued to take it. Response rates improved from 42% in the primary analysis (median exposure 8.7 months) to 54% (median exposure 28.9 months), and long-term use of everolimus appears to be safe. A meta-analysis of two randomized trials comparing 109 and 53 renal Angiomyolipoma patients treated with everolimus and placebo for 6 months, respectively, confirmed the efficacy of everolimus in reducing tumor volume by 50% or more. up (risk ratio = 24.69; P = 0.001). Everolimus is currently indicated for the treatment of adult patients with renal angiomyolipoma and tuberous sclerosis complex without immediate surgery. Some patients with hepatic hemangiomas associated with tuberous sclerosis complex have been treated with sirolimus, which has also been shown to be effective in reducing tumor volume. The role of mTOR inhibitors in patients with hepatic hemangiomas has yet to be determined, but these molecules could be used, for renal, in a palliative setting. The long-term safety profile is consistent with that previously reported and there are no new safety issues that raise concern In a retrospective Chinese series (2009-2016) of 92 patients diagnosed with histologically proven hepatic hemangioma of 2cm to 5cm in size, ultrasound-guided radiofrequency ablation after liver biopsy was used in 22/92 patient. No tumor recurrence was reported, but follow-up time was not indicated. Therefore, radiofrequency ablation can compete favorably with surgery when the hepatic hemangioma is relatively small (<5 cm) and when the patient's intrahepatic location or comorbidities are inoperable. safe.6. Arterial embolization is sometimes necessary in the presence of hemorrhagic hemangiomas
There were only eight reported cases of hepatic hemangiomas presenting as spontaneous rupture and hemorrhage. The mean size of these tumors was 8.5 cm (range: 2.5 cm to 12.5 cm). and three of them were treated with arterial embolization followed by hepatectomy allowing a definitive diagnosis of hepatic hemangioma. The primary differential diagnosis of hemorrhagic liver tumors in the liver other than cirrhosis is adenoma, which is beyond the scope of this review. Arterial embolization used in three other patients with liver hemangiomas was histologically proven (sizes: 11, 12 and 17 cm) in a US retrospective series and showed no progression. was observed after a median follow-up of 12.7 months (range, 1-36 months). The risk of spontaneous bleeding is lower for hepatic angiomas than for renal angiomyolipomas, which are usually supplied by a single vessel and are associated with aneurysms. We propose a decision algorithm for the management of liver hemangiomas

Diagnosis of hepatic hemangioma is suggested when there is fatty tissue within the solid lesion or there is wash fluid. When tumor-related symptoms are present, surgical resection is considered first. Some authors also recommend surgery in the case of hemangiomas of the epithelial type, which carries a greater risk of progression. Likewise, the association with tuberous sclerosis complex is a condition with an increased risk of malignant transformation, similar to renal hemangiomas. Follow-up is maintained despite the benign nature of the initial diagnosis because tumor activity is difficult to predict. Other possible treatment options include mTOR inhibitors, radiofrequency ablation, arterial embolization in cases of hemorrhagic rupture, and liver transplantation. The above information is for reference only about liver tumor nodes and liver hemangiomas, you should consult your doctor before deciding to use any treatment method.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Klompenhouwer AJ, Verver D, Janki S, Bramer WM, Doukas M, Dwarkasing RS, de Man RA, IJzermans JNM. Management of hepatic hemangiomas: A systematic review. Liver Int 2017; 37 (9): 1272-1280. Copyright © The Author 2017. Published by John Wiley and Sons.
Calame P, Tyrode G, Weil Verhoeven D, Félix S, Klompenhouwer AJ, Di Martino V, Delabrousse E, Thévenot T. Clinical characteristics and outcomes of patients with hepatic angiomyolipoma: A literature review. World J Gastroenterol 2021; 27(19): 2299-2311 [DOI: 10.3748/wjg.v27.i19.2299]