This is an automatically translated article.
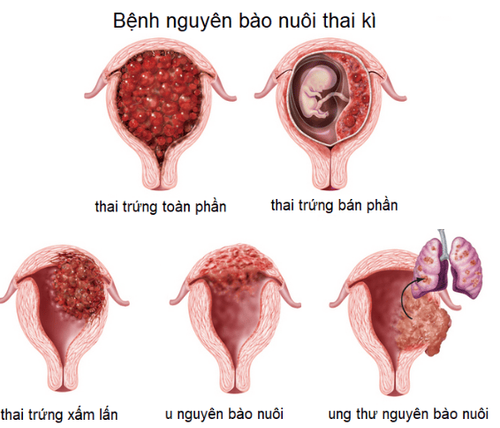
The article was consulted with Dr. Le Ngoc May - Internal Oncologist - Cancer Center - Radiation Therapy - Vinmec Times City International Hospital.Recurrent and distant metastatic trophoblastic neoplasms are life-threatening. Therefore, it is necessary to diagnose trophoblastic neoplasms early, conduct treatment and follow-up after treatment, especially in invasive cases.
1. Diagnosis of trophoblastoma
1.1. Clinical signs
To diagnose glioblastoma, your doctor will rely on your medical history, especially pregnancy, which is considered a leading risk factor for glioblastoma. In which, the majority of cases appeared trophoblastic neoplasms after total egg pregnancy (about 70%). The disease usually appears in the first 4 months after egg abortion.For functional symptoms, most of the time there are no abnormal symptoms, but sometimes there may be signs of prolonged bleeding after childbirth or abortion and metastatic symptoms such as shortness of breath, headache.
Besides, physical symptoms are expressed as follows:
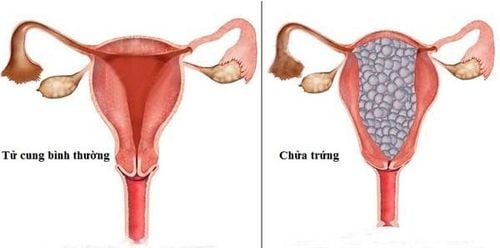
Vaginal bleeding: is the most common sign Uterus is larger than normal. Uterine density is soft, uterine contraction is poor. However, in some cases the uterus may still be normal. Nodules metastasize in the vagina, the vulva turns dark purple, mainly on the anterior part of the vagina.
1.2. Subclinical diagnosis
The subclinical signs to help diagnose glioblastoma:βhCG concentration: After pregnancy, the βhCG level increases again is an important sign to help early diagnosis of glioblastoma. When Doppler ultrasound of the uterus and uterine arteries can detect tumors in the uterine muscle, invasion of the uterine myometrium and vascular proliferation, and ultrasound also helps to detect metastases. in liver and kidney. Chest X-ray, looking for metastases in the lungs. CT scanner and MRI: help detect brain, liver, and bone metastases. A lumbar puncture if there is a suspicion of spinal cord metastases or if the patient has symptoms related to myelopathy. Biopsy of the lesions: Essential in the diagnosis but not recommended if the patient is at risk of major bleeding. In terms of pathology, it can be based on the following symptoms:
General: The uterus is larger than normal, which varies depending on the extent of the damage. The ectopic surface of the uterus becomes smooth, unless the tumor grows into the serosa or perforates the uterus. The tumor is variable in size, causing destruction of the uterine muscle to form a dark red fovea, leading to necrosis, bleeding, and pale yellow tissue areas, no follicles can be seen, but nodules can be detected. vaginal base. Microscopic examination of the tumor tissue revealed extensive necrosis, destruction of the myometrium with the presence of malignant trophoblasts (including trophoblasts and malignant monocytes). There are no vesicles, no stromal response, and almost no cell shedding.
1.3. Definitive diagnosis of trophoblastic neoplasms
The diagnosis of glioblastoma is mainly based on quantification of βhCG after egg curettage:The concentration of βhCG in the following test is higher than the previous test. The concentration of βhCG after 3 consecutive tests did not decrease significantly (decreased less than 10%). The concentration of βhCG reached over 20 000 UI/L 4 weeks after curettage. The concentration of βhCG reached over 500 UI/L after 8 weeks of egg retrieval. The concentration of βhCG reached over 5 UI/L after 6 months of egg retrieval. In addition, uterine pathology showed signs of trophoblastic neoplasms.
2. Treatment of trophoblastoma
The principle of treatment of glioblastoma is to treat it quickly as soon as the diagnosis is made.2.1. Carry out the necessary tests
Blood plot, blood group, Rh. Test liver, kidney, thyroid function. Electrolyte. X-ray through the heart. Urinalysis test.2.2. Prepare the patient
Thoroughly consult the patient's condition and relatives about the type of disease, treatment methods and possible risks. Specialist examination for accompanying diseases: Endocrine examination if there are signs of hyperthyroidism, cardiovascular examination if there is chronic hypertension. Blood transfusion in case of severe anemia. Pre-chemotherapy test the day before or on the day of chemotherapy.2.3. Uterine curettage
Pre-anesthetic or anesthetic for the patient. Intravenous infusion of 5% Glucose solution, or Ringer's Lactate, or 0.9% physiological saline. If the cervix is closed, dilate the cervix to 8-12, and aspirate the ovum with a 1-valve or 2-valve Karman tube. Clean the uterus. Use of uterotonics: Intravenous infusion of solution mixed with Oxytocin. Take specimens for histological examination (GPB) including egg tissue, placental tissue. Use antibiotics: doxycycline or cephalexin with appropriate dosage. Follow-up after hysterectomy, including general condition, uterine contraction, vaginal bleeding, abdominal pain. If within 3 days, re-examination finds that the uterus is still enlarged due to a lot of fluid retention or egg tissue, it is necessary to conduct curettage to check again.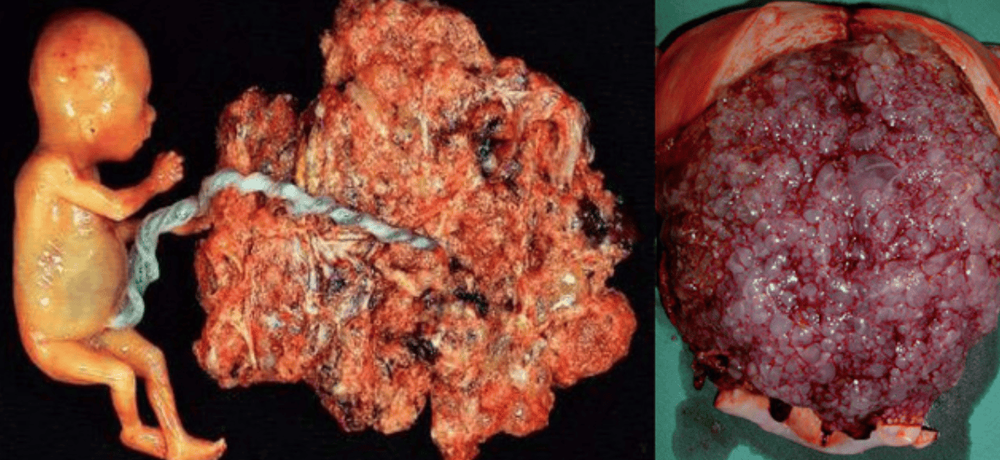
2.4. Hysterectomy
Applies to patients over 40 years old, have had enough children, have a diagnosis of high-risk pregnancy. In case of hemorrhagic, or uncontrolled heavy bleeding from the uterus.2.5. Prophylactic chemotherapy for high-risk pregnancies
Apply according to a single chemotherapy regimen in a single course.Methotrexate and Folinic Acid (MTX-FA): This is a standard monotherapy regimen with few side effects. Methotrexate is used at a dose of 1.0 mg/kg, 4 doses every other day. Folinic Acid (Leucovorin) 0.1 mg/kg dose. Leucovorin is used for 24 hours after each dose of Methotrexate. Actinomycin D daily at a dose of 1.25 mg/m2 intravenously, for 5 days, applied to patients with high liver enzymes. Methotrexate 0.4 mg/kg, intramuscularly for 5 days: This method is used for patients who do not have a long hospital stay, are in good condition, and have few side effects.
3. Follow-up after treatment for glioblastoma
3.1. Monitoring at the hospital
Monitor βhCG/blood levels every 2 weeks, until βhCG/blood is below 5mIU/ml on 3 consecutive occasions. Uterine contraction, thyroid cyst size. Vaginal bleeding, menstrual period.3.2. Follow-up after hospital discharge
Monitor βhCG/blood level once a month, continuously for 6 months. Then it can be spaced out every 2 months, for the next 6 months, and every 3 months for the next 12 months.The minimum post-discharge follow-up for low-risk pregnancies is 6 months and for high-risk pregnancies is 12 months.
Through the follow-up period after the treatment of glioblastoma, if the prognosis is good, the patient can get pregnant again. However, when there are signs of pregnancy, the patient needs to go to the antenatal clinic immediately, especially pay attention to the issue of ultrasound and the level of βhCG/blood in order to prevent repeat pregnancy.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.