This is an automatically translated article.
Severe and critical asthma attacks often occur in patients with asthma who are not monitored and do not receive preventive treatment according to guidelines. If not treated promptly, bronchial asthma can be life-threatening, even sudden death due to an asthma attack.
1. Asthma attacks
Severe and critical asthma attacks often occur in patients with asthma who are not monitored and who do not receive prophylactic treatment according to guidelines, or when acute asthma attacks are not well treated. Patients who are at risk for severe and critical asthma attacks include:
Patients with a history of severe asthma and who have been intubated or mechanically ventilated. Recently had to be hospitalized or emergency because of an asthma attack. Oral corticosteroids are often used, especially in recent cases. Inhaled corticosteroids must not be used Recently, the dose of inhaled beta-2 sympathomimetic drugs has to be increased. Have a history of mental illness or have psychological and social problems, even with sedation. The patient was not properly monitored and treated for bronchial asthma. Severe asthma attacks can appear and worsen very quickly within 2 to 6 hours by triggering factors such as:
Indoor allergens: house dust mites, molds, pet dander (cats, dogs, etc.) mice,...), cockroaches, drugs and chemicals,... Allergens outside the house: street dust, mold, pollen, ferment, chemicals, infectious factors (mainly viruses) ) or assorted smoke. Infections: mainly due to viral infections. Occupational factors: cotton dust, coal, chemicals,... Tobacco: passive or active smoking. Air pollution: emissions from vehicles participating in traffic, polluting gases and chemicals,...
2. Treatment of severe and severe asthma attacks
2.1 Principles of handling
Principles of managing severe and critical asthma attacks require expeditious, active, and correct drug use (right route, right dose). The treatment regimen for severe and critical bronchial asthma requires a combination of methods that are:
Ensure blood oxygen: Need for the patient to breathe oxygen with high flow through a nasal cannula (oxygen frame) or mask oxygen. If the patient is already on high-flow oxygen and is still severely hypoxic, mechanical ventilation is indicated. Bronchodilators: The bronchodilator of first choice is a fast-acting β2-sympathomimetic agent, the local route of administration will be the first priority (usually by nebulizer, if aerosol is not available. metered dose spray). Rapid-acting parasympathomimetic agents are also commonly used in combination with β2-adrenoceptors. Theophyllin is only considered contraindicated in patients who are poorly responsive to β2 sympathomimetic and respond well to theophyllin. Adrenalin is indicated when the above drugs must be used in high doses without effect. Corticosteroids: Systemic corticosteroids given intravenously are used in the treatment of severe asthma attacks.

Cơn hen phế quản nặng và nguy kịch thường xuất hiện trên bệnh nhân hen phế quản
2.2 Initial management of severe asthma and emergency transport
Give the patient a nebulizer 5mg immediately of a beta-2-agonist for 20 minutes, repeat the inhaler if it is not effective. Or can spray beta-2 sympathomimetic with a dose of 2-4 sprays, repeat and increase the number of sprays from 8-10 times if there is no effect. Use oral corticosteroids (prednisolone 5 mg x 6-8 tablets) or intravenous injection (methylprednisolone 40 mg). Immediately transfer the patient to the hospital. On the way of transportation, it is necessary to give oxygen to the patient at a dose of 6-8 liters / minute, continue to spray β2 sympathomimetic drugs every 10-15 minutes. A spacer should be used when administering beta-2 sympathomimetic agents.
2.3 Treatment regimen for severe asthma attacks at the hospital
Management of severe asthma attacks at the hospital according to "Treatment of severe and critical asthma attacks" of the Ministry of Health "Guidelines for diagnosis and treatment of asthma" in 2009:
First hour:
Breathe oxygen through oxygen goggles or a mask, maintain SpO2 > 90%. Bronchodilators: nebulize beta2-agonist 5 mg/ 20 minutes x 3 times in a row. Corticosteroids: methylprednisolone intravenous 40 - 80mg. Assess patient after 1 hour, if severe asthma attack has not been resolved. Next hour: Continue treatment as first hour
Oxygen ventilation through oxygen goggles or mask, maintain SpO2 > 90%. Bronchodilators: nebulized beta2-agonist 5mg for 20 minutes x 3 times in a row. Corticosteroids: if the patient has not been injected in the first hour, intravenous methylprednisolone 40 - 80mg. Besides, combined with nebulizer Ipratropium 0.5mg and intravenous magnesium sulfate 2g in 20 minutes. If severe signs in the patient have not disappeared, continue treatment. Over the next 6 - 12 hours:
Give the patient oxygen through a mask or oxygen goggles and maintain SpO2 > 90%. Bronchodilators: Continuous use of β2-agonist 5mg/time (10-15mg/hour), or continuous intravenous infusion of β2-agonist at an initial infusion rate of 0.1-0.15 Pg/kg/min , then, depending on the patient's response, increase the infusion rate every 5 minutes, 0.1-0.15 Pg/kg/min each time (up to 4mg/hour in adults). Combined with nebulizer Ipratropium 0.5 mg at a dose of 4 hours / time. Corticosteroids: methylprednisolone intravenously at a dose of 200-300 mg/24 hours, divided into 4 times. Consider indications for use:
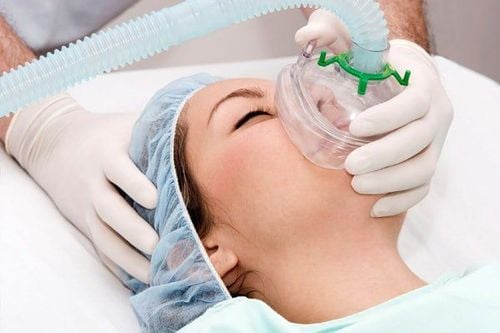
Theophylline (diaphylin) 0.24g: administered by intravenous injection very slowly (20 minutes) or mixed in 100 isotonic solutions then infused over 20 minutes. Mechanical ventilation: If after 6-12 hours, the patient has not had a good response: Continue to maintain drug treatment as above, and at the same time consider appointing adrenaline. Mechanical ventilation with non-invasive ventilation should be initiated if indications for invasive ventilation are not present. If the patient is unresponsive, endotracheal intubation is required and the patient is mechanically ventilated through the endotracheal tube. In case the patient shows signs of a serious asthma attack, before intubation, adrenaline 0.3 - 0.5 mg should be used subcutaneously and can be repeated after 5-10 minutes. Indications for endotracheal intubation and mechanical ventilation of the patient when any of the following signs appear: Signs of impaired consciousness or any other sign of a critical asthma attack. PaO2 index < 60 mmHg when the patient breathes oxygen through a mask with a reserve bag and pH < 7.30, PaCO2 > 50 mmHg. The clinical condition deteriorated rapidly. The patient is tired, the respiratory muscles are exhausted. Patients are not effective on non-invasive mechanical ventilation. Intravenous sedation in a dose sufficient to induce sleep, but not to inhibit the patient's respiratory activity (Ramsay score = 3). Stop mechanical ventilation when the patient has cleared the asthma attack, and the laboratory tests pH, PaCO2 and PaO2 are normal.
Thở oxy qua gọng kính oxy
2.4 Treatment regimen for severe asthma attacks
Squeeze the ball through the mask with a dose of 100% oxygen. Administer adrenaline 0.3 - 0.5 mg subcutaneously, may be repeated after 5 - 10 minutes. Intubation through the mouth (pay attention to sedation and/or short muscle relaxants to ensure successful intubation). Ventilation through endotracheal tube. Continuous IV infusion with a bronchodilator Adrenalin at an initial rate of 0.1 Pg/kg/min, then increased at 0.1 mg/kg/min every 2-3 minutes until responders (can add 1-1.5 mg/h in adults). Alternatively, infusion of beta-2-sympathomimetic agents can be substituted with an initial rate of 0.1 - 0.15 Pg/kg/min, and doubled every 2 - 3 minutes until the patient have response. Other drugs may also be used as regimens for severe asthma attacks. When treating a severe asthma attack, it is not necessary to follow the correct order as in the protocol. If the patient has previously had an asthma attack that has been properly managed, the next steps of management should be applied. Adrenaline is indicated when the patient has a severe asthma attack and threatens to stop the circulation, or when the patient is unresponsive to drug therapy and mechanical ventilation. When using high-dose beta-2 agonists, it is necessary to pay attention to potassium replacement for patients to avoid complications of hypokalemia.
3. Prognosis and complications
Severe or critical asthma attack depends on whether the treatment is carried out urgently and according to the right regimen. A prolonged asthma attack can worsen and become life-threatening if the patient is not treated promptly, especially if the patient is not given adequate medication or mechanical ventilation. The prognosis of a severe asthma attack will depend on the occurrence of complications. Complications that can occur after a severe and critical asthma attack such as:
Pneumothorax or mediastinum: can occur spontaneously, usually occurs with exercise, or is a complication of mechanical ventilation. Hospital infections. Water and electrolyte disorders: patients may lose water and electrolytes during respiratory exertion, hypokalemia due to high doses of sympathomimetic drugs. Some measures to prevent severe and critical asthma attacks include:
Monitoring asthma management and correct asthma prophylaxis regimen. When an acute asthma attack occurs, the patient needs to be treated aggressively, with the right method, especially for patients at risk of having a severe asthma attack. Try to limit and avoid exposure to allergens that cause asthma attacks. In summary, severe and critical asthma attacks often occur in patients with asthma who are not monitored and whose prophylaxis is not according to guidelines, or when acute asthma attacks are not well-treated. If not treated promptly, bronchial asthma can be life-threatening, even sudden death due to an asthma attack. Therefore, patients with bronchial asthma need to follow the home treatment regimen, stay away from triggers that can cause an asthma attack, and at the same time, when there are signs of a severe asthma attack, they should immediately take the patient to a medical facility. for timely intervention.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.