This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International HospitalColonic diverticulum is a common disease in the elderly, the disease often causes no symptoms, unless these diverticula become inflamed, also known as colonic diverticulitis. Therefore, patients need to pay attention, detect and treat to avoid dangerous complications.
1.What is a colonic diverticulum? Diverticula are small, bulging pouches that can form anywhere in the digestive tract, from the esophagus to the stomach, small intestine, and large intestine. However, they are usually found in the large intestine. Diverticulosis is a fairly common disease, often seen in patients over 40 years of age.
When there is a diverticulum in the digestive system, the condition is called diverticulosis. Patients may never know they exist in the body, as they rarely cause any problems, unless the diverticula become inflamed.
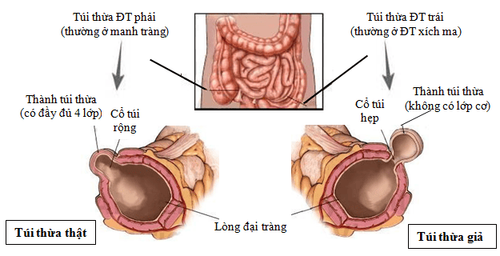
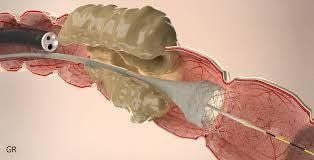
Hình 1: Hình ảnh túi thừa đại tràng
Colonic diverticula are pouch-like structures that develop in the wall of the colon, most commonly in the sigmoid and left colon, but can also involve the entire colon. When these diverticula become inflamed, it causes diverticulitis.
Diseases of colonic diverticulum:
Asymptomatic colonic diverticulum: 70% of patients have colonic diverticulum but do not show any symptoms during life. 10-25% of patients with colonic diverticulum will progress to diverticulitis and the remaining 5-10% of patients will have bleeding complications of colonic diverticulum. Colonic Diverticular Bleeding: Colic diverticulum hemorrhage accounts for about 5-10% of patients with colonic diverticulum. Gastrointestinal bleeding accounts for 40% of the causes of lower gastrointestinal bleeding and is considered a major cause of lower gastrointestinal bleeding. Diverticulitis usually occurs in the right colonic diverticulum and in 90% of cases the bleeding will stop spontaneously. Colonic diverticulitis: Colonic diverticulitis includes 2 clinical forms: simple diverticulitis (uncomplicated) and complex diverticulitis (or complicated diverticulitis). 2. Intestinal obstruction due to acute diverticulitis Diverticulitis can cause colonic strictures leading to partial or complete bowel obstruction with clinical presentation similar to other causes of obstruction, such as such as malignancy, megacolon and inflammatory bowel disease. Large bowel obstruction is thought to be caused by diverticular disease in about 10% of cases, although this number can vary considerably depending on study design. The mechanism by which diverticular disease causes large bowel obstruction is most likely due to recurrent episodes of acute diverticulitis causing fibrosis of a segment of the colon, most commonly the sigmoid colon. It should be noted that, in a small subset of patients, there will be no prior clinical diagnosis of acute diverticulitis; however, upon further inquiry, the patient may report a history of left upper quadrant pain associated with acute diverticulitis. excess bag.
3. Treatment of severe diverticulitis Treatment for severe cases associated with diverticulitis includes nasogastric tube rest to rest the bowels, antibiotics if acute diverticulitis is suspected, and the interdisciplinary diagnosis involving surgical and gastroenterology groups. Diagnostic colonoscopy may be considered if the diagnosis is uncertain and malignant obstruction must be excluded (eg, for surgical planning). This often reveals nonspecific inflammatory changes, including fissures, and may also show purulent fluid in the diverticulum. Definitive treatment previously involved emergency surgery to relieve acute intestinal obstruction but often resulted in a colectomy (stomatal opening) due to an inability to prepare the colon for surgery.
4. Placement of stents across strictures to treat intestinal obstruction due to diverticulitis Several studies have mentioned the use of colonic stents for diverticulitis-associated strictures as a bridge to surgery or palliation in patients no longer indicated for surgery. Most of the literature on this topic has combined colonic complaints associated with diverticulosis with a larger cohort of patients with other benign and malignant causes of colonic stricture.
A meta-analysis examining the technical and clinical success of self-expanding metal stents (SEMS) for benign causes of colorectal obstruction concluded that the rate of complications when Benign-obstructive stenting is too high to warrant use. The study included a large number of patients with colonic diverticulitis (66 out of 122.54%). Based on this study, the use of SEMS for severe cases associated with diverticulitis should not be considered standard therapy, but should instead be considered in a select number of cases and require multiple studies. Do more research on this topic to determine if SEMS is used (and in what patients) in the short term as a bridge to surgery or palliation in nonoperative patients.
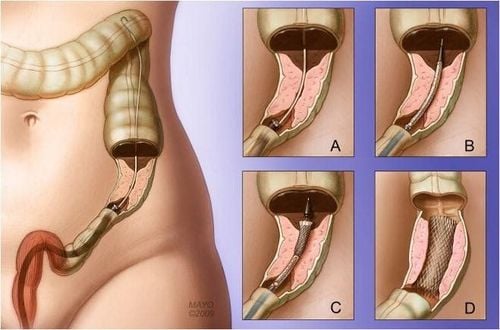
Hình 2: Stent đại tràng – dụng cụ được sử dụng để giải áp chỗ tắc nghẽn
According to the experience of many authors, colonic stenting for severe cases associated with diverticulitis is largely favorable, over 75% of patients allowed decompression and colonic preparation. After that, a colonectomy with 1 single surgery, instead of emergency colectomy, opening an stoma, then a second surgery to connect the colon (closing the anus). artificial subjects). It should be noted, however, that these strict regulations tend to be relatively rigid, and despite the advantages of the fully extended technique, indications for its application are often not seen.
Hình 3: Một trường hợp tắc nghẽn được giải áp bằng stent
4.1 Stent stenting technique An existing stent placement may be considered (although significant costs and benefits are unclear), a second stent can be inserted after dilation of the stricture of the first stent with a balloon dilatation. However, the effect is usually temporary and the narrowing after stenting tends to return. In addition, since there is essentially no mucosal abnormality (i.e. cancer) to which the stent can easily be attached, there may be a complication of stent migration out of the narrow site. Therefore, it is recommended to use clips to clamp the stent at the distal end with multiple segments to minimize the risk of stent migration in both directions.
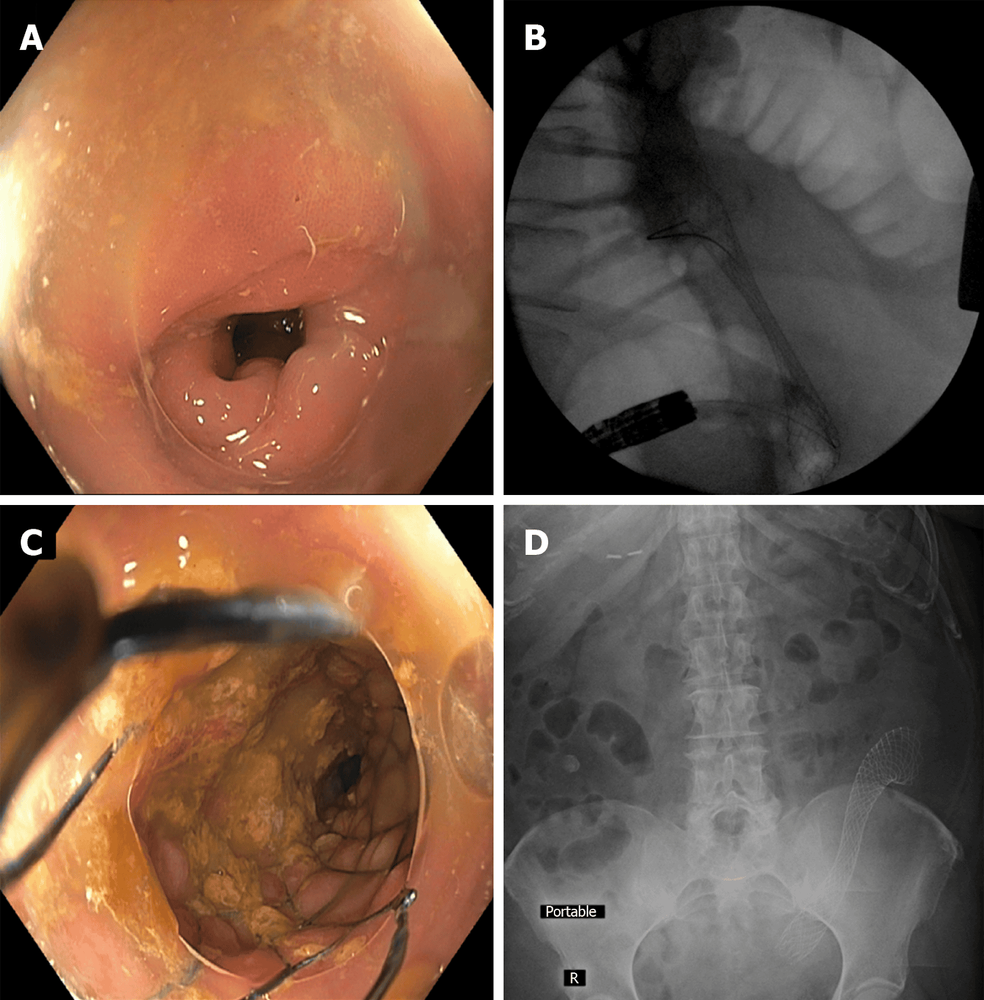
Hình 4: Đặt stent đại tràng trong trường hợp hẹp đại tràng liên quan đến viêm túi thừa.
A: Sigmoid stenosis due to diverticulitis associated with diverticulitis
B: Fluorescence imaging of colonic self-expanding metal stent deployment with significant waist circumference
C: endoscopic image after stent
D: Post-procedural abdominal X-ray showed the stent in good position and significant dilatation. This treatment may allow successful bowel preparation and colectomy 1 instead of emergency colectomy with a temporary colostomy and a second colostomy.
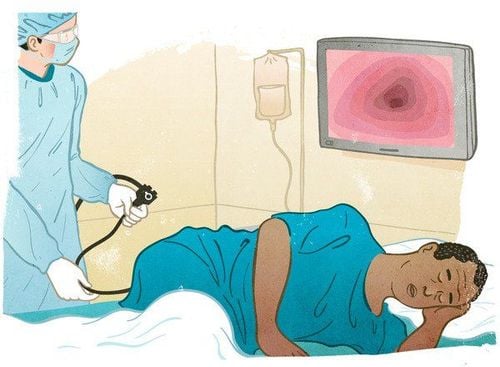
5 Follow-up colonoscopy after diverticulitis Current guidelines recommend diagnostic colonoscopy after resolution of acute diverticulitis if a colonoscopy has not been performed recently. Colonic wall thickening on imaging may also result from processes other than diverticulitis, such as ischemia, inflammatory bowel disease, or malignancy. The rationale for follow-up colonoscopy is to avoid underdiagnosing any of these conditions, especially malignancy. This is usually done 6-8 weeks after improvement of acute diverticulitis in patients who have not had a colonoscopy in the previous 1-2 years, although the optimal timing of colonoscopy remains unclear.
Some problems associated with colonoscopy in patients with diverticulitis
Colonoscopy is useful in the diagnosis of asymptomatic colonic diverticulitis and is an effective means of treatment in bleeding colonic diverticulum. However, in diverticulitis, colonoscopy is considered a relative contraindication, because the inflation process increases intraluminal pressure and may rupture the acutely inflamed diverticulum, causing inflammatory complications. Peritoneal . On the other hand, similar to colonoscopy, flexible bronchoscopy only examines the inside of the colon, while the manifestation of diverticulitis mainly occurs on the outside of the gastrointestinal tract, so endoscopy does not provides a wealth of information for the diagnosis of diverticulitis. However, colonoscopy has a role in monitoring proliferative diseases after treatment of diverticulitis. In cases where the standard adult endoscope cannot pass through the sigmoid colon, because the colon is fixed after the inflammatory process, using a small diameter colonoscope for children can help the process. easier colonoscopy
Diverticulosis can increase colonoscopy difficulty due to narrowing of the colon lumen, angulation, colonic spasms, and difficulty opening the lumen during endoscopic gas injection. The standard technique with the adult bronchoscope may not be sufficient to achieve cecaloscopy. Using a pediatric bronchoscope, more suitable for endoscopy, may be beneficial. The addition of a transparent cap at the tip of the bronchoscope may also be helpful. Instead of using air blows, pumping water during a colonoscopy (water pump endoscopic technique) can help move through the narrow sigmoid colon. In more difficult cases, fluoroscopy may be used to help guide the colonoscope. Of course, positioning the patient and pressing directly into the abdomen are always useful adjuncts.
The distribution and severity of diverticular disease and colon-related changes are different in each patient. Therefore, many authors should use a detailed description of the location and extent of diverticular disease when writing each laparoscopic report. This will provide richer information for clinicians caring for patients with diverticulitis, diverticulitis, or diverticulitis in the future.
Authors around the world have come up with improved techniques to treat diverticulitis, treatment techniques for severe cases related to diverticulitis, new data reported potentially promising for the use of colonic stents as a palliative and bridging measure for surgery, but further research is needed on the utility and optimal application for the patient. Follow-up colonoscopy after an episode of acute diverticulitis continues to be recommended in those who have not had a colonoscopy in the previous 1–2 years, despite the optimal timing and true efficacy of colonoscopy. in this context is still uncertain and it may be beneficial to do further research. Finally, a variety of techniques have been implemented to maximize the safety and success of the procedure in patients with endoscopic dense metastasis.
Currently, Vinmec International General Hospital performs diagnostic and treatment techniques for colonic diverticular disease with Olympus CV 190 endoscope, NBI function (Narrow Banding Imaging - endoscope with narrow light frequency band) ) results in clear mucosal pathology analysis images to detect abnormal mucosal lesions at an early stage, thereby making the treatment more effective and safe. The examination is always carried out by a team of experienced doctors and experts, well-trained in domestic and foreign environments. Therefore, customers can completely rest assured with the gastrointestinal endoscopy service at Vinmec International General Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.