This is an automatically translated article.
When the way to the duodenum is blocked, surgery is needed to make an anastomosis between the stomach and the jejunum loop. If gastric stenosis occurs after surgery or for other reasons, it can be treated under the guidance of digital angiography with background erasure.
1. Overview
There are many different diseases that narrow the upper gastrointestinal tract (including: stomach, duodenum and first part of jejunum). The most common conditions are:
Benign/malignant stenosis of the gastrojejunum after surgery; Chronic peptic ulcer disease Stomach cancer ; Pancreatic cancer ; Invasive duodenal tumor (rare). Up to now, the method of dilation and stenting of the stomach - duodenum under flexible endoscopic guidance has been widely applied. However, this technique is still deeply invasive, especially in patients who are exhausted or uncooperative, or require general anesthesia. There are even cases of unsuccessful implementation because the bronchoscope cannot pass through the narrow position.
Treatment of re-circulation for the gastrointestinal tract with interventional radiology has been applied in many countries around the world. Advantages of the treatment of gastric stenosis under the guidance of digital angiography with background erasure are:
Minimally invasive; Does not require general anesthesia; The tools and vehicles are very small in size, so they are likely to succeed when going through a narrow place; Less complications; Good support in cases where surgery is no longer indicated or has had surgery before.
2. When should treatment under the guidance of digital angiography erase the background?
2.1. Point
Gastrocolic stenosis at the anastomosis: Benign stenosis after surgery, recurrent tumor causing malignant gastrocolic stricture; Malignant strictures of the stomach, duodenum or jejunum: Gastric-duodenal cancer but no longer indicated for tumor resection, pancreatic head or invasive cholangiocarcinoma, and some cancers metastasis ; Benign stenosis due to other diseases: Ulcer, chronic gastritis - duodenum.
2.2. Contraindications
Peritonitis (the lining that covers the organs in the abdomen); Patients with systemic infections; Gastrointestinal perforation from any cause; Progressive damage to the esophagus from burns or cancer.

Bệnh nhân viêm phúc mạc chống chỉ định
3. Preparation steps
3.1. Executor
Specialist doctors and radiology technicians; Support medical team; Nursing staff; Anesthesiology medical staff (if the patient is no longer able to cooperate).
3.2. Vehicle
Digital background removal angiography (DSA); Film, film printers and image storage systems; Lead vest and protective apron, X-ray shielding.
3.3. Medicine
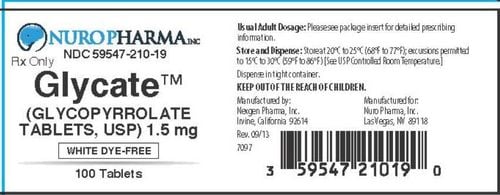
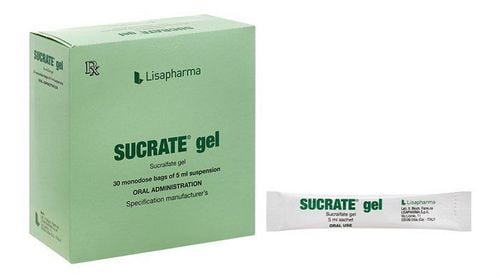
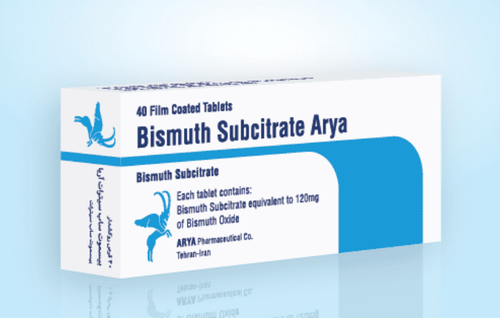
Local anesthesia and general anesthesia (if indicated); Water-soluble Iodine Contrast Contrast; Limit spasms of the digestive tract; Antiseptic solution for skin and mucous membranes.
3.4. General medical supplies
Syringes of all kinds 5 - 10 - 20ml; Distilled water or physiological saline; Surgical caps, gowns, gloves and masks; Sterile interventions: Knives, scissors, tongs, metal bowls, bean trays and trays; Cotton wool, medical gauze and surgical tape; Medicine box and first aid kit for contrast dye accidents.
3.5. Special medical supplies
Kim Chiba soft tissue aspiration; Catheter set into the lumen of the vessel; Standard conductor size 0.035 inch; Hard conductor 0.035 inch long (260 - 300cm); Cobra 4-5F angiography catheter; Balloon angioplasty; Pressure pump; Bracket (stent).
3.6. Patient
Be explained by the doctor about the procedure to coordinate well during the implementation; Need to fast before 6 hours, drink less than 50ml of filtered water; The patient lies supine in the intervention room; Install a monitor to monitor the following indicators: breathing rate, pulse, blood pressure, electrocardiogram and oxygen saturation SpO2 ; Disinfect the skin and then cover with a sterile towel; If the patient is too excited, can't lie still, give a dose of sedation.
3.7. Test form
Inpatient medical records; Indication card to carry out the procedure; X-ray film, CT Scan, or MRI if available.
4. Steps to take
4.1. Narrow location review
Insert the catheter and guide through the mouth - esophagus into the stomach to reach the narrowing site; Withdraw the lead wire; Inject water-soluble contrast material to assess the location and extent of gastric stricture.
4.2. Approaching a narrow location
Continue to thread the guide wire through the narrow position under the guidance of the enhanced X-ray screen; Insert the tube through the gastrocolic stenosis under the guidance of a guide wire; Inject the contrast agent through the catheter to determine the extent, location, and length of the narrowing.
4.3. Angioplasty and stent placement at the narrow site
Insert the rigid conductor into the conduit through the narrowing; Use a balloon dilatation of the gastrocolic stricture through a rigid conductor; Place and release the bracket through the stiff wire.
4.4. End of the trick
Take contrast dye to check the circulation from the stomach to the duodenum and jejunum; Withdraw all leads and catheters.

Sau thực hiện thủ thuật, bệnh nhân cần được theo dõi chặt chẽ
5. Complications and treatment
The treatment of gastroesophageal stenosis under the guidance of digital angiography erasing the background is evaluated as successful when:
Regarding position: The stent is located in the correct position of the gastroesophageal stenosis, the upper and lower ends cover the occlusive stricture. at least 1cm. About function: When pumping drugs from upstream, there is circulation to downstream. The lumen of the gastrointestinal tract is still not more than 30% narrow. There is no escape of the contrast agent out of the digestive tract into the abdominal cavity, or the retroperitoneal space. Note, in the process of performing the technique, there is also a risk of rare complications such as:
Stent slip: Occurs when choosing a bracket that is not suitable for the degree of narrowing; Intestinal obstruction: Due to the rack sliding downstream, or fibrous, undercooked food caught in the stent; Esophageal perforation: Emergency surgery; Gastrointestinal bleeding: Need to monitor and treat medically. In case the bleeding does not stop on its own, endoscopic intervention is used. In summary, digital erasure angiography (DSA) will intervene from within the vascular lumen, with the advantage of minimally invasiveness without the need for open surgery. One of the common applications of this method is to guide dilation and stenting of the gastrointestinal tract, which helps to treat gastric stenosis without drugs, as well as to limit surgical complications.
Vinmec International General Hospital is one of the general hospitals that ensures the function of examination, prevention and treatment of many diseases. Received the trust of many customers, now Vinmec has been and continues to bring standard medical equipment system with modern medical services, a team of qualified doctors and nurses with many years of experience. Seniority in the profession will bring optimal treatment results, satisfying customers.
Customers can directly go to Vinmec Health system nationwide to visit or contact the hotline here for support.