This is an automatically translated article.
The article is advised by BSCK II Pham Thi Son - Neurologist - Department of Medical Examination & Internal Medicine, Vinmec General Hospital Hai Phong.And Specialist I Do Van Manh - Emergency Resuscitation Doctor - Emergency Resuscitation Department - Vinmec Ha Long International General Hospital.
Treatment of ischemic stroke with fibrinolytics within the first three hours of the onset of symptoms increases the odds of being non-disabled or minimally disabled by 30%. On average, 1 out of every 8 patients treated promptly with thrombolysis will have a normal recovery.
1. Methods of treatment of cerebral infarction
Cerebral infarction accounts for about 85% of stroke cases. In order to successfully treat cerebral infarction, the issue of time and treatment method plays a decisive role.
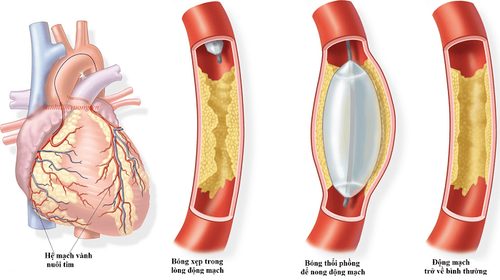
Currently, two methods of treating cerebral infarction are injection of fibrinolytic drugs and thrombectomy with mechanical instruments. The golden time for thrombolytic injection is < 4.5 hours from the onset of symptoms, while mechanical thrombectomy is < 6 hours from the onset of symptoms.
In the article, we will go into depth on the method of treating cerebral infarction with fibrinolytic drugs.
2. What are thrombolytics?
Thrombolytic drugs (thrombolysis) have a role in dissolving thrombosis (blood clots that block the flow of blood vessels in the brain and cause a stroke). Thrombosis is caused by fibrin. During thrombolysis, plasmin is a substance that destroys firbin to form soluble degradation products. The recombinant tissue plasminogen activator rTPA (as Alteplase) has a selective effect on fibrin, converting plasminogen to plasmin, dissolving blood clots. This is the only drug approved by the United States (FDA) for use in the treatment of acute ischemic stroke within 3 hours of the first symptoms appearing.

3. Efficacy of fibrinolytic drugs
The fibrinolytic drug rTPA (Alteplase) has the role of reducing disability rate and increasing the ability to recover movement of patients after cerebral stroke. To be effective, patients need to be treated with thrombolytic drugs within 3 hours of the onset of symptoms. Therefore, the patient should be taken to the hospital as soon as possible.
The proportion of patients without disability, or minimal motor paralysis increases by more than 30% if treated early with thrombolytic drugs in the first 3 hours after the onset of symptoms. 13% of patients can recover function after three months. One out of every three patients treated during the "golden period" will have better results than if they did not receive timely treatment. In addition, one out of every eight patients will be able to return to a normal life.
4. Indications/Contraindications to the use of thrombolytic drugs:
Indications: Patients >= 18 years old. The time from onset of stroke to taking the drug is not more than 3 hours, can be extended to 4.5 hours. Diagnosis of acute ischemic stroke with 4 < NIHSS < 22. No brain hemorrhage on CT or MRI. Contraindications: Stroke onset symptoms >4.5 hours or uncertain timing. Onset of convulsions. No unenhanced CT scan of the skull or evidence of bleeding on CT of the brain. Cases of stroke suggestive of subarachnoid hemorrhage despite a normal CT scan. Cranial CT image: Large cerebral infarction (> 1/3 hemisphere). The patient had a major neurological deficit (NIHSS score > 22). Injury or progressive bleeding. History of stroke, severe head trauma, myocardial infarction, or brain surgery in the last 3 months. There is a history of cerebral hemorrhage. History of gastrointestinal bleeding within 21 days History of major trauma or major surgery within 14 days. Lumbar puncture or arterial puncture in a non-compressible site for 7 days. Have intracranial pathology (arteriovenous malformation, aneurysm). There is an abnormality in blood sugar (< 50 mg/dl or > 400 mg/dl). Platelet count < 100,000 mm3. Uncontrolled BP (systolic BP > 185 mmHg or diastolic BP > 110 mmHg). Recent anticoagulation with an INR > 1.5 s. Blood sugar <2.8 mmol/l or > 22.2 mmol/l.
5. Thrombolytic drugs
Streptokinase : A synthetic protine from C ß - Hemolytic streptococci with a half-life of 16-90 minutes, Streptokinase acts through binding to plasmin to form a complex capable of breaking down plasminogen into plasmin. Currently, due to the increased risk of bleeding, Streptokinase is no longer used.
Urokinase is a glycoprotein that can be cleaved from renal tissue, with a half-life of 9-12 minutes. Unlike Streptokinase, Urokinase is an endogenous substance, so it is not susceptible to hypersensitivity reactions.
rtPA (Recombinant Tisue Plasminogen Activator) (brand name Alteplase) is synthesized by endothelial cells and circulates in low concentrations in the blood with a half-life of 3-8 minutes. rtPA has a specific binding site on the platelet membrane and is 100-fold more potent when activated at the firbin-plasminogen complex. It is currently the only FDA-approved thrombolytic agent for the treatment of acute ischemic stroke.
Some other substances: Reteplase, Tenecteplase, Destmoteplase... have a longer half-life and in some initial trials promising results. However, it is still in the testing process.

6. Process of treating cerebral infarction with fibrinolytic drugs
6.1 Treatment of thrombolysis with intravenous thrombolytics: As recommended, the fibrinolytic agent Alteplase (Actylyse 50mg/50ml vial) is used at a dose of 0.9mg/kg (maximum dose 90mg), of which 10 % injected intravenously in 1 minute. The remaining 90% is given as a continuous intravenous infusion over 1 hour. After that, the patient was transferred to the intensive care unit or the stroke unit for monitoring. Computed tomography again after 24 h and antiplatelet therapy may be initiated thereafter if no bleeding is observed. 6.2 Thrombolytic therapy with arterial thrombolytic drugs Arterial thrombolytic therapy has the advantage that the drug is concentrated in high concentrations in the area where the thrombus is located, with little systemic effect; at the same time can directly evaluate the revascularization process. However, this is a complicated technique and can only be performed in a few specialized facilities. Therefore, the proportion of patients undergoing arterial thrombolytic therapy is much lower than that of the intravenous route.
After performing DSA, approaching the site of occlusion, inject rtPA diluted 0.2mg/ml directly into the occlusion site. Scan for direct assessment of revascularization.
7. Side effects when treating cerebral infarction with fibrinolytic drugs
Possible complications after injection of other capsular thrombosis such as:
Brain bleeding: Symptoms of headache, nausea/vomiting, worsening of consciousness. Computed tomography scan showed bleeding in the brain. The rate of cerebral hemorrhage accounted for 6.4% (1 out of 16 cases had cerebral hemorrhage.
Extracranial bleeding: Bleeding in the eye, bleeding in the stomach, bleeding in the teeth...
Some reactions were too high. Other sensitivities: Rash, urticaria, bronchospasm, angioedema, hypotension...
Treatment of cerebral stroke with fibrinolytic drugs only works within the first 4.5 hours maximum. When detecting symptoms of cerebral infarction, it is necessary to quickly bring the patient to the nearest hospital or medical facility for timely emergency treatment. Thrombolytic drugs are opening up hope and opportunities for stroke patients. The sooner the patient is treated with this method, the faster the recovery will be without leaving any sequelae.
Currently, Vinmec International General Hospital is applying fibrinolytic therapy to emergency patients who have had a stroke, with a treatment success rate of over 90%, this result is real. It means a lot to the patient.
With modern imaging equipment, CT perfusion results are available within 7 minutes and performed routinely. To achieve the above successes, it is impossible not to mention the contribution of experienced doctors at Vinmec along with a system of modern equipment to support and a very strict medical examination and treatment process. Completely feel secure when being treated here.
If you are not sure if you have a stroke, you should have a stroke screening. Currently, Magnetic Resonance Imaging - MRI/MRA is considered a "golden" tool to screen for brain stroke. MRI is used to check the condition of most organs in the body, especially valuable in detailed imaging of the brain or spinal nerves. Due to the good contrast and resolution, MRI images allow to detect abnormalities hidden behind bone layers that are difficult to recognize with other imaging methods. MRI can give more accurate results than X-ray techniques (except for DSA angiography) in diagnosing brain diseases, cardiovascular diseases, strokes,... Moreover, the process MRI scans do not cause side effects like X-rays or computed tomography (CT) scans.\
Vinmec International General Hospital currently owns a 3.0 Tesla MRI system equipped with state-of-the-art equipment by GE. Healthcare (USA) with high image quality, allows comprehensive assessment, does not miss the injury but reduces the time taken to take pictures. Silent technology helps to reduce noise, create comfort and reduce stress for the client during the shooting process, resulting in better image quality and shorter imaging time. With the state-of-the-art MRI system With the application of modern methods of cerebral vascular intervention, a team of experienced and well-trained neurologists and radiologists, Vinmec is a prestigious address for stroke risk screening and screening. reliable goods.
In the past time; Vinmec has successfully treated many cases of stroke in a timely manner, leaving no sequelae: saving the life of a patient suffering from 2 consecutive strokes; Responding to foreign female tourists to escape the "death door" of a stroke;...
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.