This is an automatically translated article.
The article is professionally consulted by Master, Doctor Pham Van Hung - Interventional Cardiologist - Department of Medical Examination & Internal Medicine - Vinmec Danang International HospitalMyocardial infarction is a dangerous disease caused by a sudden blockage of a blood vessel supplying the heart. When the heart muscle is completely deprived of blood supply, the muscle in that area will die, causing severe chest pain symptoms.
1. Warning signs of a heart attack
A heart attack is a sudden blood clot that blocks a coronary artery (the blood vessel that feeds the heart). This phenomenon prevents blood from flowing to the heart muscle and causes part of the heart muscle to die. Blockage of large blood vessels can cause the heart to stop or it can cause a deadly arrhythmia.Many people have only very mild chest pain or discomfort below the breastbone. These symptoms may be transient and then return to normal immediately. People who have a heart attack may not even notice this symptom until other painful symptoms occur.
The most obvious warning symptom is chest pain : Chest pain is usually in the middle of the breastbone and lasts for a few minutes. The pain may come and go and come back again. The pain makes the person feel like something is pressing on the chest, stabbing pain, or feel suffocated.
The pain can also appear in other locations such as in the back, on the neck, on the jaw or in the epigastrium. Shortness of breath is often accompanied by chest pain. Some other symptoms may also be accompanied by cold sweats, vomiting or mild headache.
2. Subjects prone to myocardial infarction
Men over 45 and women over 50 are at high risk of having a heart attack. However, young people can also have a heart attack, but less often. People who have had a heart attack in the past are more likely to have another heart attack. People with a family history of an early myocardial infarction such as a father or brother who had a myocardial infarction under the age of 55 and a mother or sister who had a myocardial infarction under the age of 65. Patients with diabetes have a similar risk of myocardial infarction as patients with a history of myocardial infarction. People with high risk factors such as dyslipidemia, high blood pressure, smoking, obesity, and lack of physical activity are the most likely to have a heart attack.
3. The principle of urgency in the treatment of myocardial infarction

The death rate from myocardial infarction in the world used to be about 30-40%, today it has decreased to 20% and in the last 4 decades it has decreased to about 6 -10%: all thanks to the urgency treatment promotion.
Furthermore, immediate treatment is needed because reperfusion with angioplasty will have a much better outcome if performed within the first 12 hours, or reperfusion with thrombolytics will be very effective. high if the drug is administered as soon as possible (within the first 2 hours) and not late after the 6th hour.
Recently there has been an opinion that it is permissible to use thrombolytics to dissolve thrombosis even after 6-12 hours even up to 24 hours when the following conditions are excluded: necrosis is progressing (manifesting continued chest pain), ST segment (electrocardiogram) is still elevated, and cardiac enzymes are continuously elevated.
4. Use of thrombolytic drugs
Once the diagnosis of myocardial infarction has been confirmed, the rule is: do not wait for the results of the "cardiac marker (cardiac enzyme)" test, but promptly prescribe as soon as possible the use of thrombolytic drugs with venous line. The effect of thrombolytic drugs is to dissolve thrombosis, so fibrinolysis is classified as "acute coronary reperfusion" treatment.
4.1 Absolute contraindication History of intracranial hemorrhage. Aneurysms, cerebral arteriovenous shunts. History of intracranial tumor. Ischemic stroke < 3 months. Transient ischemic attack < 6-12 months. Aortic dissection. Severe trauma <3 months. Severe uncontrolled hypertension (>180/110 mmHg). Disorders of clotting factors. History of hemorrhagic stroke. Acute pericarditis. Pregnant < 5 months. 4.2 Relative contraindications Gastric ulcer, enteritis. Internal bleeding (2 - 4 weeks). Ischemic stroke > 3 months old. Prolonged cardiopulmonary resuscitation (>10 min) causes trauma. Surgery < 10 days; neurosurgery < 2 months; major surgery < 3 months. History of intraocular bleeding (proliferative retinopathy; ophthalmic surgery). Menorrhagia, heavy bleeding. Bleeding. Amniocentesis < 24-48 hours. Other invasive procedures < 10 days. Gastrointestinal/urinary-genital bleeding <10 days. Chronic cavernous lung disease. 4.3 Possible complications Intracranial hemorrhage 0.7% - 0.9%. This risk doubles in people >75 years of age with severe hypertension. 4.4 Signs of fibrinolytic drugs achieving treatment results Chest pain is gone. The ST segment is no longer elevated. There may be transient appearance of ventricular tachyarrhythmias (due to reperfusion). 4.5 If results are not achieved (60 – 90 minutes after initiation of fibrinolytics) the following presentation will occur: Persistent chest pain. Decrease in ST elevation by only < 50%.
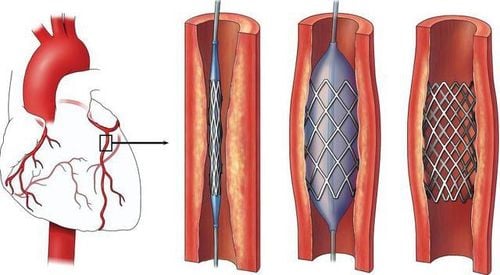
5. Indications for cardiovascular intervention - Heart attack surgery
Coronary intervention in case of acute myocardial infarction without fibrinolysis:
Myocardial infarction has been more than 6 - 12 hours Contraindications to thrombolytics. If you take fibrinolytic drugs, you may not be able to survive the risk of major life-threatening complications:
Threatening or in cardiogenic shock. Heart failure gets worse. New left bundle branch block appears. After fibrinolysis is not effective
Use of fibrinolytics, if 60-90 minutes does not achieve results (still persistent chest pain, ST-segment elevation reduction of only <50%), urgent intervention is needed. coronary artery.
6. Comparison of results between angioplasty and thrombolytic drugs
In terms of myocardial resuscitation, coronary intervention is not inferior to fibrinolytic drugs. In general, patients feel that coronary intervention is better than fibrinolysis. The results in terms of reducing myocardial infarction and mortality are better with coronary intervention than with conventional thrombolytics. Coronary intervention also avoids the threat of intracerebral bleeding complications (especially in patients 60 - 75 years old). When considering between drugs and cardiovascular intervention, there are many aspects, but the basic thing is to choose how to timely coronary reperfusion.
7. Combination of drugs and cardiovascular intervention
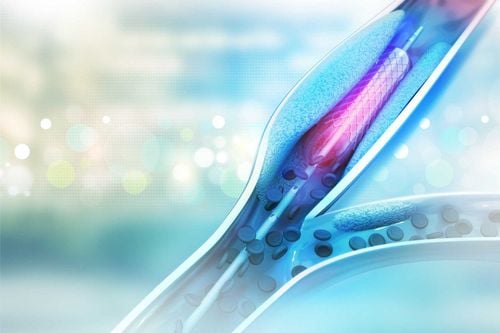
Use half a dose of fibrinolytic drugs and then switch to coronary intervention immediately. After fibrinolysis (whole dose) 2-7 days, all patients received additional treatment with coronary intervention, termed delayed coronary intervention. After fibrinolysis (whole dose) 2 days (48 hours), if the patient presents with myocardial ischemia, then choose to have additional coronary intervention. Nowadays, after fibrinolytic therapy, coronary interventional procedures always include stenting (supporting frame) to completely reduce coronary re-stenosis after 6 months in combination with antithrombotic therapy.
It can be seen that the examination, screening and diagnosis of cardiovascular diseases is very important, including urgent cardiovascular emergency measures. The method of fibrinolytic therapy for patients with acute myocardial infarction at Vinmec International Hospital has a success rate of over 95%. Thrombolytic drugs are used for patients with myocardial infarction with indications under the guidance and close monitoring of cardiologists, experienced and modern equipment.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.