This is an automatically translated article.
Article written by BSCK I Tran Ngoc Thuy Hang, Emergency Department, Vinmec Central Park International General Hospital
Acute respiratory failure is a dangerous disease that causes many serious complications such as sepsis, multi-organ failure and death if not treated early. So how to treat ARDS, what treatment methods are there?
Treatment of ARDS includes:
Treatment of severe hypoxemia Treating the cause Supportive treatment
1. Supportive treatment
Very few patients with acute respiratory failure die from respiratory failure alone. The majority of deaths are related to the primary cause of ARDS or to subsequent complications such as sepsis , multiple organ failure , .
The supportive treatment of patients with ARDS requires meticulousness and ingenuity, including: flexible use of sedatives and muscle relaxants; Hemodynamic monitoring, nutritional support, blood sugar control, active assessment and treatment of hospital-acquired pneumonia if present, prevention of deep vein thrombosis and gastrointestinal bleeding.
Sedation – analgesia: useful in improving patient ventilatory cooperation, while reducing oxygen consumption requirements. Choosing a drug depends on the characteristics of each patient, for example, an anxious patient will choose a benzodiazepine group, . . . Usage: usually injected intermittently. Objectives: patient is awake, comfortable, cooperative or mildly sedated with RASS (Richmond Agitation – Sedation Scale) 0 or -1; In some cases of patients with severe lung damage, asynchronous mechanical ventilation can maintain deeper sedation. Attention should be paid to the potential side effects of sedatives and analgesics. Muscle relaxant - neuromuscular blockade: beneficial in improving oxygenation, however the undesirable effect is persistent neuromuscular weakness. Neuromuscular blocking agents are only used in patients with ARDS when indicated: asynchronous mechanical ventilation, anti-machine ventilation, emergency intubation, tremor associated with hypothermia after circulatory arrest, convulsive conditions malignancy, . . . Nutritional support: patients with ARDS have an intense catabolic metabolism because they need to compensate for the energy loss due to catabolism and modulate the metabolic response to stress, reduce oxidative cell damage, and modulate the metabolic response. beneficial immune response. Enteral feeding is recommended when possible. Enteral feeding reduces the risk of endovascular infection, reduces gastrointestinal bleeding due to gastric buffering, and maintains the intestinal mucosal barrier, thereby reducing microbial invasion through the intestinal wall. Note the patient's head position when feeding to reduce the risk of ventilator-associated pneumonia.

Thuốc an thần kèm thở máy có hiệu quả trong điều trị bệnh ARDS
Nosocomial pneumonia is quite common among ARDS patients. A prospective study of 30 patients with severe ARDS showed a 60% incidence of nosocomial pneumonia. The first episode of nosocomial pneumonia occurred on average within the first 10 days after the onset of ARDS. With abnormalities, it is difficult to diagnose nosocomial pneumonia in patients with ARDS based on radiographic abnormalities and initial clinical signs. Guidelines for the prevention of ventilator-associated pneumonia should be applied for prevention, early diagnosis, and treatment. Glucocorticoids are indicated in patients with ARDS in the following cases: Underlying conditions with indications for glucocorticoid treatment such as severe sepsis, treatment-resistant; . . . . Moderate, severe ARDS in the relatively early stage (within the first 14 days from onset) failed standard therapy (PaO2/FiO2 ratio <200 despite recommended initial therapy including volumetric ventilation) Low dose) Glucocorticoids: Methylprenisolone 1mg/kg/day for 21-28 days Dexamethasone 20mg once daily for 5 days, then 10mg once daily for the next 5 days.

Chụp X-quang phổi giúp chẩn đoán bệnh ARDS
2. Management of hypoxemia
ARDS is severe hypoxia. Measures to help increase arterial oxygen saturation include:
Increasing the concentration of oxygen in the inhaled air: most patients with ARDS require high-concentration oxygen. Prior to intubation, the patient required oxygen via a mask or a high flow nasal cannulae. Immediately before and after intubation, it is necessary to maintain a FiO2 (distribution of oxygen in inhaled air) of 95-100% to maintain an adequate SaO2. FiO2 should then be gradually reduced to 50-60% as safely possible with a goal of PaO2 55-80mmHg or SaO2 88-95% Fluid management: as is known, early ARDS has an accumulation of interstitial fluid. due to imbalance between hydrostatic pressure and colloidal pressure, causing pulmonary edema. Therefore, it is necessary to limit the fluid even though the patient does not have circulatory overload. The goal in fluid management: CVP (central venous perssure) < 4 mmHg or PAOP (pulmonary artery occlusion pressure) < 8 mmHg, however this goal is practically difficult to achieve. . Some preliminary data suggest that combination therapy with albumin infusion and diuretics may improve fluid balance, oxygenation, and hemodynamics. Supportive measures to improve SaO2 include prone ventilation and strategies to reduce oxygen consumption
Reduced oxygen consumption: causes of increased oxygen consumption include fever, anxiety, pain, and respiratory muscle strain, so SaO2 can be improved with the combination of antipyretic, antipyretic, and antipyretic drugs. relax, relieve pain, relax muscles. Improve oxygen delivery: Oxygen supply is decided by the formula: DO2 = 10 x CO x (1.34 x Hgb x SaO2 + 0.003 x PaO2) (DO2 oxygen supplied, CO, cardiac output, Hgb concentration Hemoglobin, SaO2 arterial blood oxygen saturation)
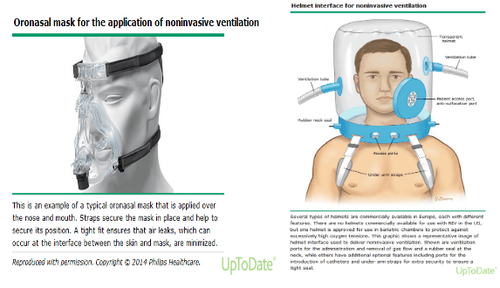
Therefore to improve oxygen delivery target Hgb 7-9g/Dl; Because transfusion of erythrocytes increases the risk of developing ARDS, transfusion of erythrocytes is indicated when HGB is < 7g/Dl. Support mechanical ventilation: depending on the degree of respiratory failure to choose the mode of respiratory support: Non-invasive ventilation: applicable to mild ARDS cases, no indications for intubation trachea immediately, hemodynamic stability, easy control of oxygenation. Non-invasive modes of ventilation: via branch canule; masks, helmets.
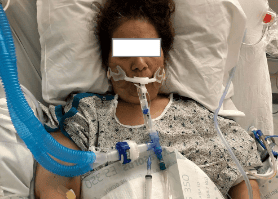
Invasive ventilation: through endotracheal or tracheostomy: Mechanical ventilation strategy in patients with ARDS: pulmonary protective ventilation with low tidal volumes, setting PEEP according to FiO2. The goal of ventilation is to maintain SaO2 88-95%; PaO2 55-80 mmHg. As soon as the first symptoms of the disease appear, you should immediately go to a reputable medical facility for examination and treatment. Vinmec International General Hospital is a high-quality medical facility in Vietnam with a team of highly qualified medical professionals, well-trained, domestic and foreign, and experienced.
A system of modern and advanced medical equipment, possessing many of the best machines in the world, helping to detect many difficult and dangerous diseases in a short time, supporting the diagnosis and treatment of doctors the most effective. The hospital space is designed according to 5-star hotel standards, giving patients comfort, friendliness and peace of mind.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.













