This is an automatically translated article.
The article was written by Dr. MSc Nguyen Thuc Vy - Doctor of Radiology, Department of Diagnostic Imaging - Vinmec Nha Trang International General Hospital.Thoracic outlet syndromes (TOS) refer to a group of clinical syndromes caused by compression of the brachial plexus or the subclavian vessels as they pass through the superior thoracic fissure.
1. Anatomy
The thoracic outlet is an anatomical area in the lower part of the neck defined as a group of three compartments between the collarbone and the first rib through which several important neurovascular structures pass. These structures include the brachial plexus, the subclavian artery, and the subclavian vein. Compression of this area causes a range of symptoms that can include pallor in the upper extremities, paresthesias, weakness, muscle atrophy, and pain.TOS classification is based on the pathophysiology of symptoms with subtypes including neurogenic (nTOS), venous (vTOS), and arterial (aTOS). Furthermore, each of these subtypes may be related to congenital, traumatic, or acquired causes. Examples of congenital etiology include the presence of an abnormal cervical or first rib. Acquired causes may be related to vigorous, repetitive sports or work-related activity.
The thoracic outlet includes the space from the supraclavicular fossa to the axillary fossa. Symptoms of TOS arise from compression of the brachial plexus nerves, the subclavian artery and vein, and the axillary artery and vein.
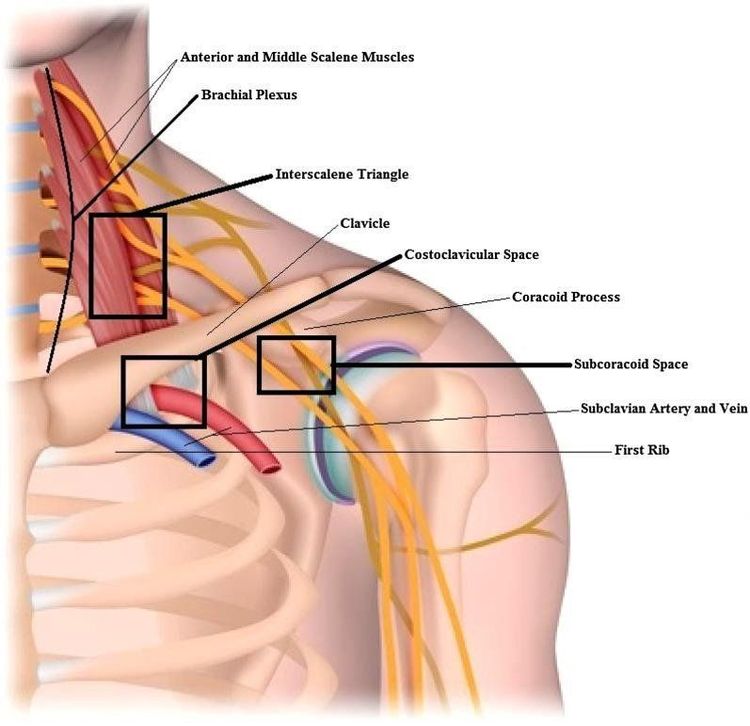
The anatomic compartments of thoracic outlet syndrome include:
Interscalene triangle : bounded by the anterior trapezius muscle, the posterior medial trapezius muscle, and the 1st rib posterior inferior, contains the brachial plexus and the subclavian artery. Costoclavicular space: bounded anteriorly by the subclavian muscle, posteriorly by the 1st rib and anterior stepladder, and above by the clavicle, containing the brachial plexus, subclavian artery, and inferior vena cava blow. Subcoracoid space: bounded anteriorly by the pectoralis minor, posteriorly by ribs 2-4, superiorly by the cranium, containing the brachial plexus, axillary artery and axillary vein.
2. Causes of thoracic outlet syndrome
Multiple mechanisms produce the characteristic pathology of TOS, including trauma, repetitive motion, and anatomical variations.Injury most commonly occurs in the case of high-speed motor vehicle accidents. Hemorrhage, hematoma, or displaced fracture can put direct pressure on nerves or blood vessels. Collar fracture is a recognized cause. In addition, scarring after the initial lesions can also be the cause of symptoms.
Repetitive movements can lead to muscle hypertrophy causing compression. Venous TOS can also occur after repetitive motion. Paget-Schroetter disease, also known as "exertional thrombosis," involves thrombosis of the axillary or subclavian veins following repetitive arm movements.
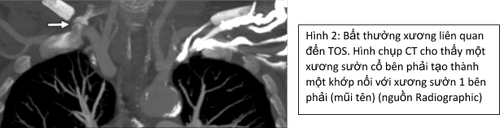
Numerous anatomic variations can cause TOS: cervical rib, 1st rib abnormality, clavicle, C7 transverse process elongated,.... The estimated prevalence of cervical rib is 1–2 % of the general population, but the majority of cases with cervical ribs are asymptomatic. Patients with cervical ribs have a higher risk of nTOS, with 20% of nTOS cases due to the presence of cervical ribs alone. The presence of cervical rib is also a risk factor for the development of arterial TOS as it can compress the subclavian artery, causing stenosis or aneurysm. Congenital variations in the musculature have also been reported to be common causes, for example the anterior trapezius muscle may attach abnormally to the 1st rib and cause compression of the vascular bundle in the triangle of the ladder.
Benign or malignant tumors of the base of the neck, such as those in the upper lobes of the lung (pancoast tumors), can invade and compress the brachial plexus and blood vessels.
3. Epidemiology
Due to the multiplicity of etiologies and the lack of expert consensus for a definitive diagnosis, the true incidence of TOS is difficult to distinguish. Several articles report an incidence of 3–80/1000.Neurological TOS (nTOS) is by far the most common, accounting for approximately 95% of cases. Venous TOS accounts for 3-5% of cases and arterial TOS is 1–2%.
Neurological TOS is more common in women. Women between the late teens and early 60s are more commonly affected by nTOS, often affecting one side rather than the other.
Arterial TOS usually affects mainly one side, affects both sexes equally, and usually affects young adults.
Venous TOS also tends to affect one side and is more common in men than women. Because of its involvement with repetitive upper limb activity, vTOS is more common in younger individuals and usually affects the dominant hand.

4. Clinical manifestations
Timely recognition of the signs of TOS is important to prevent complications such as ischemic necrosis, pulmonary embolism, and permanent nerve damage. The clinical presentation depends on the compression structure and degree of compression.Nerve TOS: the most common (90-95%), compression of the brachial plexus leads to pain, paresthesia, and numbness of the upper extremities. Venous TOS: Second most common, subclavian vein compression causes swelling and pain in the upper extremities and can lead to venous thrombosis (Paget-Schroetter syndrome), which may present with symptoms of venous compression. intermittently in the absence of thrombosis (Mccleery syndrome). Arterial TOS: the rarest form (less than 3% of cases), compression of the subclavian artery causes ischemia with cold sensation, pallor, pain, paresthesia, and decreased pulse in the upper extremities. Symptoms of vascular bundle injury may be compounded and these are aggravated by certain arm positions and manipulations, especially with overhead manipulation.
5. Diagnosis
Diagnosis includes clinical examination, electromyography, electrophysiology to evaluate nerve conduction and imaging methods including Doppler vascular ultrasound, neck-thoracic x-ray to evaluate anatomical variations. of the cervical basal bone, CT and MRI with contrast agent.Contrast-enhanced CT is useful for evaluating thoracic spine abnormalities and for detecting arterial and venous abnormalities such as stenosis/occlusion, thrombosis, aneurysm/pseudoaneurysm, and evaluation of the collaterals. .
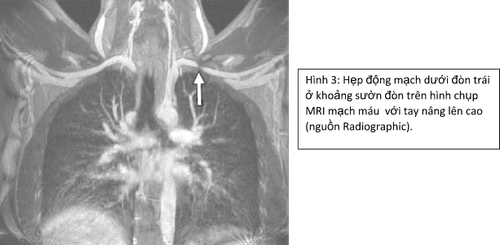
MRI is useful in patients with neurologic TOS syndrome, particularly in evaluating the brachial plexus and surrounding structures. MRI can evaluate bone and soft tissue abnormalities, fat loss around the brachial plexus in the raised position, and brachial plexus edema.
In addition, computed tomography (CT) or MRI scans provide additional anatomical detail needed for surgical planning.
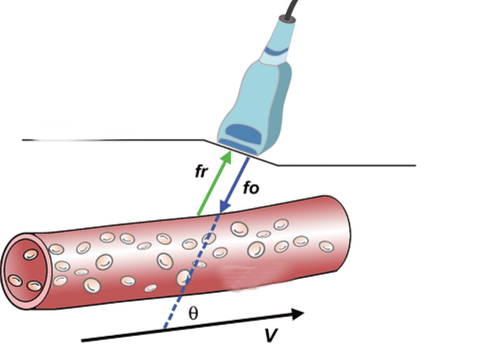
For vascular TOS, vascular Doppler ultrasonography has high sensitivity and specificity, is noninvasive, and is inexpensive, and should be the initial imaging test of choice.
Image taken with patient's arm in both elevated and neutral position with arms extended for comparison.
6. Treatment
Treatment strategies depend on the etiology of TOS. Initial treatment of neurologic TOS includes conservative measures such as medication and rehabilitation methods. Conservative treatment and physical therapy for neurologic TOS should last for at least 4–6 months before considering surgical intervention.However, for patients with arterial or venous TOS, the initial intervention is usually surgery to prevent acute thromboembolic events. A trial of direct vascular catheter anticoagulation and systemic heparin therapy may be attempted first in patients with arterial or vascular TOS in mild upper extremity ischemia. .
For patients with cervical ribs, treatment is reserved for symptomatic patients, as the presence of cervical ribs exists in 0.5% of the population but only a small percentage develops symptoms. .
Vinmec International General Hospital is one of the hospitals that not only ensures professional quality with a team of leading medical doctors, a system of modern equipment and technology. The hospital provides comprehensive and professional medical examination, consultation and treatment services, with a civilized, polite, safe and sterile medical examination and treatment space.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: radiopaedia.org, NCBI, pubs.rsna.org