This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Advanced endoscopic imaging in inflammatory bowel disease has seen a major innovation revolution in the past 10 years, including both live and virtual chromoscopy. The results of dye-stained colonoscopy are highly anticipated and may open new avenues for diagnostic and therapeutic strategies in inflammatory bowel disease.
1. Role of magnifying endoscopy and dye-based staining endoscopy in the diagnosis of Crohn's disease
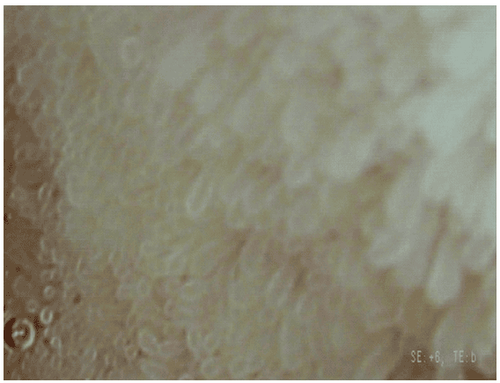
Magnifying endoscopy uses a movable lens to vary the magnification up to 150x, thus allowing mucosal surface characterization (eg, grading the surface pattern of colonic polyps). as suggested by Kudo et al in 1996).
2. Classification of endoscopic staining
Staining endoscopy is divided into dye-based staining endoscopy (DBC) and dye-free staining endoscopy (DLC). Dye-free endoscopy also includes optical staining endoscopy and virtual optical staining endoscopy. The basic principle of endoscopic photochromic staining is to enhance the detail of the mucosa and/or the submucosal vascular network with the use of different dyes or endoscopic/optical color schemes and calculator. Contrast enhancement of mucosal surfaces often leads to improved detection of subtle lesions.
3. Substances and instruments used in endoscopic staining
Dye-based endoscopy using different staining agents is divided into absorbers (Lugol, methylene blue, toluidine blue, and cresyl violet), contrast agents (carmine indigo, acetic acid) and dyes. reactive staining (congo red, phenol red). The dye is mainly used via standard spray or catheter catheters used in biliary ERCP procedures.
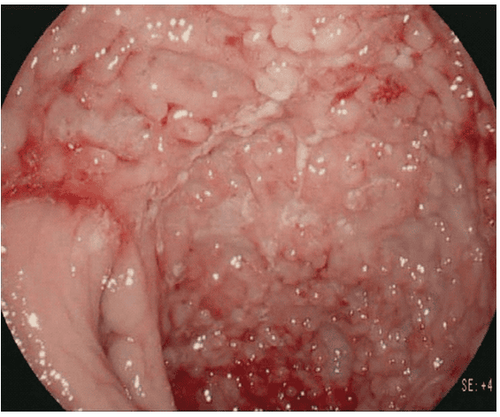
Various studies have shown the potential of staining endoscopy to enhance the detection of precancerous and cancerous lesions in inflammatory bowel disease. A randomized, controlled trial evaluated whether staining endoscopy using 0.1% methylene blue could facilitate early detection of intraepithelial neoplasia and CAC in UC. Stained colonoscopy allows a more accurate diagnosis of the extent and severity of inflammatory activity in ulcerative colitis than conventional colonoscopy and significantly improves the early detection of intraepithelial neoplasia and carcinoma. CAC in patients with ulcerative colitis.
Another colonoscopy study evaluated endoscopic pancolonic staining with 0.1% indigo carmine to detect dysplasia in ulcerative colitis. Untargeted biopsies did not detect dysplasia in 2904 biopsies, whereas the targeted biopsy procedure with staining endoscopy required fewer biopsies (157) and detected nine dysplastic lesions. These results were confirmed in a large prospective trial including 102 patients with chronic colitis using methylene blue appendectomy. Focused biopsies with dye spray showed significantly more dysplasia than random biopsies and more than with targeted dye injection.
A meta-analysis of 6 randomized controlled trials that evaluated the diagnostic accuracy of staining colonoscopy for the detection of dysplasia in ulcerative colitis. The meta-analysis demonstrated a composite sensitivity of 83.3%, specificity of 91.3%, and a diagnostic odds ratio of 17.5. It is concluded that staining endoscopy has moderate to high sensitivity and high diagnostic accuracy for detecting dysplastic lesions in ulcerative colitis.
4. The role of magnified staining endoscopy
Hurlstone and colleagues analyzed high-magnitude staining colonoscopy in ulcerative colitis as a reliable tool for disease severity assessment. 325 patients were included prospectively, and magnified endoscopy was significantly better than conventional colonoscopy for predicting the extent of disease in vivo. This same group prospectively analyzed indigo carmine-assisted high-magnification endoscopic staining for the detection and characterization of intraepithelial neoplasia in UC.
Intraepithelial neoplastic lesions were significantly more detected in the magnified endoscopy group than in the control group. Furthermore, endoscopic staining increased the number of flat lesions with intraepithelial neoplasia detected compared with controls. Another group studied pitting patterns in the rectal mucosa by magnifying colonoscopy as a marker of recurrence in patients with already well UC. Multivariable proportional hazard modeling analysis showed that magnified endoscopy surface pattern analysis could significantly predict disease recurrence in patients with sedated ulcerative colitis. These results were also confirmed by Watanabe and colleagues.
Endoscopy with staining and targeted biopsies of suspected lesions is a more effective method of surveillance in inflammatory bowel disease than multiple untargeted biopsies alone. Magnified staining endoscopy improves detection of precancerous and neoplastic mucosal changes. Magnified endoscopy has the potential to predict recurrence in patients with asymptomatic disease.
5. Coloroscopy without dyes
Dye-free staining endoscopy is divided into optical pigmentoscopy including narrow band imaging (NBI; Olympus, Tokyo, Japan) and virtual pigmentary endoscopy including iscan (Pentax, Tokyo, Japan) and Fujinon intelligent color enhancement (FICE; Fujinon, Tokyo, Japan). While NBI is based on optical filters inside the light source of the endoscope, narrowing the spectral transmission bandwidth, thereby enhancing vascularity, i-scan and FICE use digital post-processing to estimate the spectrum. calculated to produce better tissue contrast.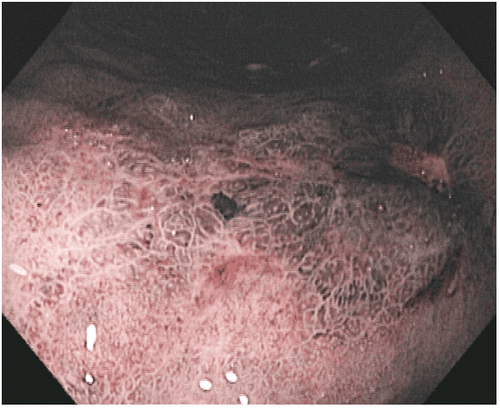

Recently, Vden Broek and colleagues performed a randomized crossover trial in which UC patients underwent both inflammatory bowel disease white light colonoscopy and high definition (HD) in randomized order. course. It was shown that NBI did not improve cancer detection in patients with ulcerative colitis compared with HD colonoscopy. In addition, the NBI proved unsatisfactory in distinguishing cancerous from noncancerous mucosa. The same group evaluated the value of three-way endoscopic imaging for surveillance in ulcerative colitis.
6. Conclusion
Advanced endoscopic imaging in inflammatory bowel disease has seen a major innovation revolution in the past 10 years, including both live and virtual chromoscopy. Using capsule endoscopy or balloon-assisted small bowel endoscopy, endoscopists can now assess the entire small intestine and perform endoscopic therapies in a place that has never been visited before. via. Recent efforts have been made to introduce molecular imaging in inflammatory bowel disease by highlighting inflammatory cells and specific receptors. The results of these trials are highly anticipated and may open new avenues for diagnostic and therapeutic strategies in inflammatory bowel disease.
Vinmec International General Hospital is a prestigious address trusted by many patients in performing diagnostic techniques for digestive diseases, diseases that cause chronic diarrhea, Crohn's disease... Along with that, at Vinmec Hospital, screening for gastric cancer and gastric polyps is done through gastroscopy with Olympus CV 190 endoscope, with NBI (Narrow Banding Imaging) function for The imaging results of mucosal pathology analysis are clearer than conventional endoscopy, detecting ulcerative colitis lesions, early gastrointestinal cancer lesions... Vinmec Hospital with facilities With modern quality and equipment and a team of experienced experts, always dedicated to medical examination and treatment, customers can rest assured with gastroscopy and esophagogastroduodenoscopy at Vinmec International General Hospital. .
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:
Ullman TA, Itzkowitz SH. Intestinal inflammation and cancer. Gastroenterology. 2011;140(6):1807–1816. [PubMed] [Google Scholar] Farraye FA, Odze RD, Eaden J, Itzkowitz SH. AGA technical review on the diagnosis and management of colorectal neoplasia in inflammatory bowel disease. Gastroenterology. 2010;138(2):746–e4. [PubMed] [Google Scholar] Günther C, Martini E, Wittkopf N, et al. Caspase-8 regulates TNF-alpha , epithelial necroptosis and terminal ileitis. Nature. 2011;477(7364):335–339. [PMC free article] [PubMed] [Google Scholar] Neumann H, Vieth M, Langner C, Neurath MF, Mudter J. Cancer risk in IBD: how to diagnose and how to manage DALM and ALM. World Journal of Gastroenterology. 2011;17(27):3184–3191. [PMC free article] [PubMed] [Google Scholar] Rutter MD, Saunders BP, Wilkinson KH, et al. Thirty-year analysis of a colonoscopic surveillance program for neoplasia in ulcerative colitis. Gastroenterology. 2006;130(4):1030–1038. [PubMed] [Google Scholar] Helmut Neumann, Klaus Mönkemüller. Advanced Endoscopic Imaging for Diagnosis of Crohn's Disease, Gastroenterol Res Pract. 2012; 2012: 301541.














