This is an automatically translated article.
The article is professionally consulted by Master, Doctor Mai Vien Phuong - Gastroenterologist - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.Autoimmune gastritis (VDDTM) is an atrophic gastritis of the gastric mucosa, mainly focusing on the body and gastric aneurysm, due to the appearance of antibodies against the parietal cells of the stomach and intrinsic factor, which can lead to destruction. stomach lining, resulting in anemia and vitamin B12 deficiency, even leading to stomach cancer. This pathology has so far received little attention and is easily missed.
1. Role of blood tests
Anti-parietal cell antibodies: Finding specific antibodies in VDD helps to screen and confirm the diagnosis more effectively. The most commonly used antibodies are the anti-parietal cell antibody (APCA). Antibodies against intrinsic factor. According to a study, anti-toxin antibodies have a sensitivity and specificity of 81% and 90%, respectively, while anti-intrinsic factor has 100% specificity but a poor sensitivity of 27%. Quantification of gastrin levels 17 also helps to assess the state of increased gastrin secretion from G cells due to decreased secretion of gastric juice. Diagnosis by combining tests of anti-parietal cell antibodies, anti-internal factor, gastrin 17, pathological results. Increased gastrin levels can also be seen in some other diseases such as Zollinger Ellison syndrome, so for differential diagnosis, it is possible to measure the concentration of acid produced in the stomach. In patients with chronic atrophic gastritis, the level of gastric acid produced was as low as <5 mEg/hour while in patients with Zollinger Ellison it was 10 mEg/hour. In addition, it is necessary to exclude cases with obstruction or disturbance of gastric motility by endoscopy and other methods of exploration. Pepsinnogen (PG) I, II: Measuring concentration and using PGI/PGII index to coordinate diagnosis. PGI is produced by the primary cells of the gastric aneurysm body while PGII is produced by both primary and glandular cells in the entire gastric mucosa. Therefore, in autoimmune gastritis, there will be a decrease in PGI concentration and PGI/PGII index <3. Patients with macrocytic anemia should have vitamin B12, homocysteine and methylmalonic acid measured. Their values can change over time but in some cases the values are still within the normal range. Serum iron: helps to comprehensively assess the patient's anemia problem.

2. The role of histopathology (consider the specimen under the microscope)
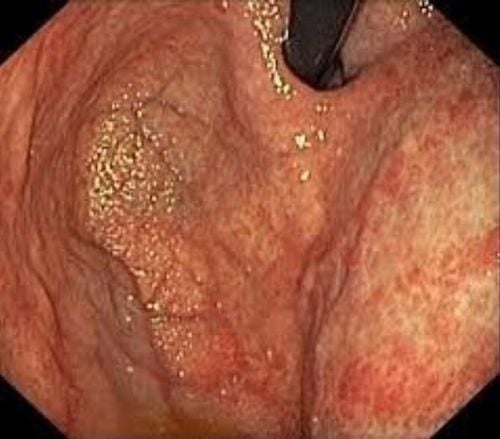
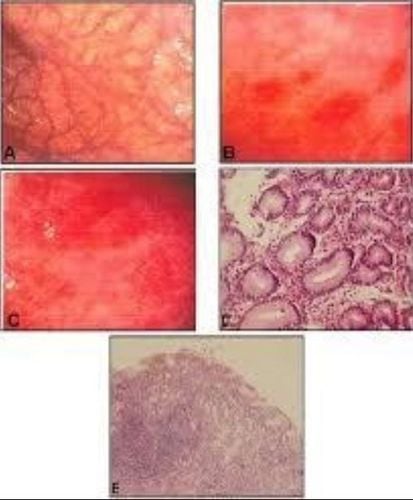
Macroscopic assessment is mainly based on gastric specimens. In the early stages there is not much marked change in the mucosa, but as atrophic inflammation progresses, the lining of the body becomes thinner, the mucosal folds are flattened. In addition, small nodules (hyperplastic polyps, pseudopolyps, adenoma polyps, carcinoid tumors...).
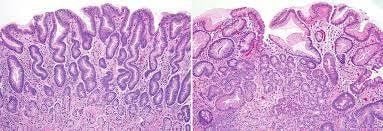
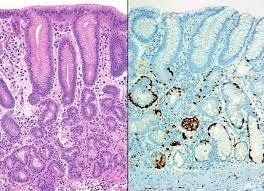
Microscopically, autoimmune gastritis is a focal atrophic lesion localized to the body with intestinal metaplasia, pancreatic cystic cell metaplasia, or pheochromocytoma. In the absence of HP co-infection, the antral mucosa is normal or shows only mild reactive inflammation.
Changes on microscopic lesions can be divided into three stages:
Early stage: characterized by infiltration of lymphocytes and plasma cells into the mucosal area of acid secretion, increasing the thickness of the membrane. bottom. This process may involve both eosinophils and mast cells. In addition, destruction of gastric acid-secreting glands by lymphocytes began to be observed in each region. These early features are often nonspecific, so the pathologist may be suspicious and recommend additional serological tests for anti-parietal cell and anti-parietal cell antibodies. interior. In the second stage: there is a stronger infiltration of lymphocytes, plasma cells, obvious atrophic inflammation of the acid-secreting glands, the thickness of the mucosa is usually unchanged or sometimes reduced. go. The intestinal metaplasia or pseudopyloric metaplasia can be clearly observed. At this stage, if only the atrophic inflammatory lesion is evident in the body biopsy fragment while the biopsy piece from the antrum is normal, the pathologist can confirm the diagnosis of VTE. The final stage is characterized by significant reduction or complete loss of gastric acid secretion glands, with the formation of hyperplastic or inflammatory polyps. Pseudopyloric dysplasia, intestinal metaplasia, and cystic cell metaplasia of the pancreas are widespread and a thickening of the muscularis mucosa may be seen. Occasionally, hyperplastic lesions of the ECL cells can be seen. The use of immunohistochemistry will make the diagnosis easier.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
ReferencesDao Viet Hang-Dao Van Long (2018), “Autoimmune gastritis”, Autoimmune diseases – gastrointestinal allergies, Medical producer. Carmel R(2996) Prevalence of undiagnosed pernicious anemia in the elderty Arch Intern Med, 156 1097-200. 3. Andres E, Serraj K (2012), Optimal management of pernicious anemia. JBlood Med, 3:97-103. 4. S Strickland RG, Mackay IR (1973), A reappraisal significance of the nature and of chronic atrophic gastritis. Am J Dig Dis, 18:426-40. 5. Park JY, Lam-Himlin D, Vemulapalli R (2013). Review of autoimmune metaplastic atrophic gastritis. Gastrointest Endosc, 77(2):284-92. 6. Kulnigg-Dabsch S.(2016), “Autoimmune gastritis”, Wien Med Wochenschr 166(13-14):424-430