This is an automatically translated article.
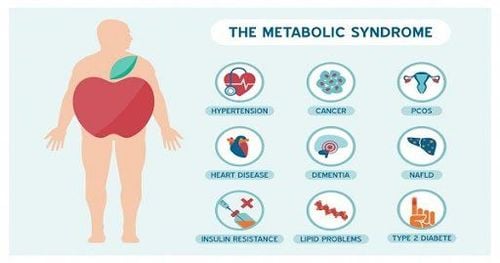
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General HospitalBased on numerous epidemiological studies, metabolic changes such as insulin resistance, diabetes mellitus, and metabolic syndrome are frequent comorbidities in patients with hepatitis C infection, in contrast to controls. The rationale for this association is still not fully understood but it may be attributed to the presence of liver disease, metabolic features such as obesity, or the inflammatory process caused by HCV infection.
1. Role of HCV in the regulation of insulin signaling pathways
HCV has been found to regulate insulin signaling pathways although the exact molecular mechanism of HCV-mediated insulin resistance is still not fully understood. In two experimental studies in mouse models, the HCV core protein was found to play a key role in the development of insulin resistance, particularly through the PA28γgene-dependent pathway. HCV genotypes 1, 2 and 4 and genotypes 1 and 4 were found to have higher insulin resistance than genotypes 3 and genotypes 2 and 3, respectively. Oxidative stress and proinflammatory cytokines have also been found to play a role in de novo insulin resistance.2. Patients infected with hepatitis C are prone to metabolic syndrome
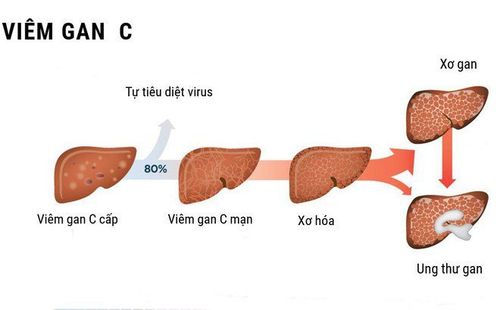
Disruption of glucose and lipid metabolism associated with insulin resistance leads to progression of hepatic steatosis and development of diabetes mellitus. Among subjects with chronic liver disease, the prevalence of diabetes in patients with hepatitis C infection before treatment varied from 13.6% to 67.4%, which is higher than reported rates. reported in people with other etiologies, such as chronic hepatitis B. Furthermore, a case-control study demonstrated that the presence of hepatitis C infection was associated with a more than 11-fold increased risk of diabetes during a follow-up period of 9 years. Diabetes appears to have a two-way relationship with HCV, with the latter causing insulin resistance while diabetes mellitus is associated with a more positive course of HCV-related outcomes such as fibrosis. progression, and an increased risk of cirrhosis and HCC. All of the above conditions make patients infected with hepatitis C more susceptible to metabolic syndrome. However, because hypolipidemia due to HCV infection, which did not conform to traditional diagnostic criteria, a special form of metabolic syndrome known as hepatitis C metabolic syndrome was identified.
3. Beneficial effects of antiviral therapy on insulin resistance in long-term HCV responders
There is frequently evidence of a beneficial effect of antiretroviral therapy using interferon-based regimens on insulin resistance in long-term HCV responders. Thompson et al, who studied 1038 non-diabetic patients, concluded that insulin resistance was significantly reduced in HCV-genotype 1 responders but not in HCV-genotype 1 nonresponders or people with genotype 2 or 3 regardless of treatment outcome. This finding was independent of any change in BMI. Similar findings were also reported in a prospective study. In Virahep-C, a prospective multicenter study, improvement in the assessment of the homeostasis model for insulin resistance (HOMA-insulin resistance) was observed 24 weeks after completion of treatment in those HCV genotype 1 patients had insulin resistance prior to treatment. However, Aghemo et al, who enrolled 384 non-diabetic patients with HCV genotypes 1 and 4 did not show any difference in HOMA-insulin resistance values between baseline and 24 weeks after sustained virological response.
All of the above findings indicate that longer follow-up may be needed to better assess glucose metabolism disturbances after HCV viral clearance with interferon-based regimens, particularly in genotyped HCV patients 1. Paradoxically, in a head-to-head comparison of 178 subjects with HCV genotypes 1 and 4 between interferon-based antiviral therapy and DAAs to assess metabolic outcomes, there was a significant increase in HOMA- insulin resistance in people already taking an interferon-based regimen.
4. Antiretroviral therapy is also thought to reduce the incidence of post-SVR hyperglycemia and diabetes.
In addition to its effect on insulin resistance, antiretroviral therapy is also believed to reduce the incidence of post-SVR hyperglycemia and diabetes mellitus. Interferon-based regimens have been studied extensively, and they are generally associated with a reduced incidence of diabetes mellitus in non-diabetic hepatitis C-infected patients after HCV eradication. However, several studies have highlighted the beneficial role of achieving SVR in reducing glucose metabolism abnormalities associated with HCV infection. Other studies failed to detect any significant differences between treatment responders and nonresponders.
5. Correlation between HCV clearance through interferon-based regimens and incidence of hyperglycemia
Despite these conflicting results, a meta-analysis of seven studies investigating the correlation between HCV clearance via interferon-based regimens and the incidence of hyperglycemia demonstrated that the A sustained virological response was associated with a lower risk of hyperglycemia [odds ratio 0.49, 95% confidence interval (CI): 0.42–0.58]. Heterogeneity between studies was minimal, indicating a reliable outcome. On the other hand, the use of DAA to eradicate viruses has not been well studied. Studies of the incidence of diabetes in non-diabetic patients have shown less glucose disturbances in long-term responders. In a retrospective study conducted in the United States, 5,127 HCV-positive non-diabetic subjects were enrolled to investigate how response to HCV treatment influenced subsequent diabetes risk.
6. SVR has a markedly lower risk of developing diabetes compared with treatment failure
The authors found that people who achieved SVR had a markedly lower risk of developing diabetes than those who failed treatment. Two studies investigated the effects of DAAs in patients with known diabetes. One illustration shows improvement in glycemic status after viral treatment, whereas there is no difference in glycosylated hemoglobin between pretreatment and posttreatment values.
Importantly, one-third of the patients in the second study required increased antidiabetic therapy during antiretroviral therapy. Further long-term prospective studies are still needed to address the current dilemma of changes in insulin resistance associated with antiretroviral therapy.
Conclusions Extrahepatic manifestations including cardiometabolic conditions are commonly seen in patients infected with hepatitis C. Data for these conditions after HCV eradication are inconsistent. To further determine the extent of the association between sustained virological response and extrahepatic manifestations and to understand the precise mechanism of how antiviral therapies affect these extrahepatic manifestations, it is necessary to have large prospective studies with long follow-up.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.