This is an automatically translated article.
Extradural hematoma, medically known as Extradural Hematoma, occurs when there is a hematoma in the middle cavity of the skull and the outer protective membrane of the brain, also known as the dura mater.
1. Causes of epidural hematoma
The most common cause of acute epidural hematoma is primarily severe head trauma. During trauma, the skull fractures and tears blood vessels and causes them to leak, causing a hematoma in the epidural space. A large amount of blood will put pressure on the brain. If not treated in time, the patient can suffer brain damage, which is life-threatening.
2. Symptoms of acute epidural hematoma
Symptoms of acute epidural hematoma are mostly expressed in the patient's problems or gradual loss of consciousness. However, according to the cases that have occurred, this symptom does not happen often, because most of the time after the patient wakes up from the trauma, he will feel quite normal. After that, the disease will get worse and this is when the patient feels the most obvious signs, specifically:
Severe headache; Sleepy; Nausea or vomiting; Becoming confused and weak in one arm/leg; Sometimes convulsions occur; Unable to talk normally (difficulty talking).

Ngưởi bệnh xuất hiện tình trạng nhức đầu dữ dội
Anyone who has had a head injury and has the above symptoms and signs is better off seeing a doctor right away. Extracranial CT scan helps us to visualize the epidural hematoma.
Acute epidural hematomas are more common in younger people than in older people (about 6 in 10 people with epidural hematomas are under the age of 20). Doctors have shown that in the elderly, the periosteum (dural) layer is more firmly attached to the skull, making it less likely that hematoma between the skull and the dura mater will occur. In contrast, in young people, the dura mater is not firmly attached to the skull.
People who drink too much alcohol are also more likely to develop an epidural hematoma due in part to the fact that they are more likely to fall. Acute epidural hematoma is also less common in women than in men.
3. Treatment of acute epidural hematoma
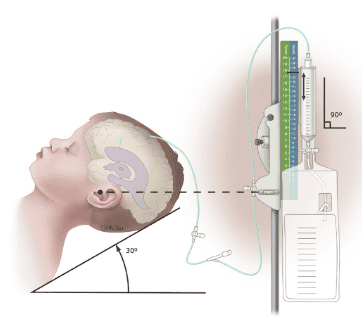
3.1. Diagnostic findings This is an acute condition, the injured person needs to be taken to the emergency hospital. The doctor will check the patient's level of consciousness, tremors in the arms and legs, and examine the eyes to diagnose the degree of pressure of the hematoma on the skull.
Medical procedures used to diagnose an acute epidural hematoma include:
Blood tests: pinpoint the cause and avoid confusion; Head CT scan; X-rays to diagnose injuries in other areas.

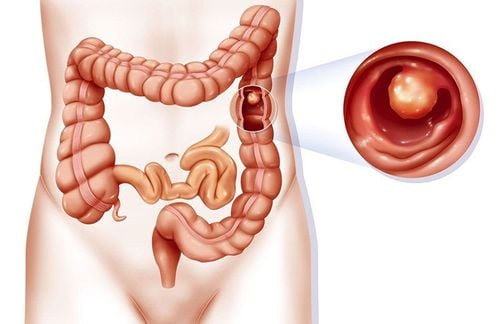
Tụ máu ngoài màng cứng cấp tính
3.2. Treatment of acute epidural hematoma If the epidural hematoma is small and has no specific symptoms, the physician will simply monitor the patient's condition and not interfere too much with the treatment methods. because the clot can reabsorb on its own.
The first priority when treating an acute epidural hematoma is stabilizing the condition. For example, when a patient has high blood pressure or difficulty breathing, you need to intervene in the immediate treatment. If the pressure on the skull is increased because of the large hematoma, the doctor will appoint the patient to need surgery or medication.
3.3. Disease prevention To prevent acute epidural hematoma , it is important to protect yourself from head injuries, especially for young children:
Wear helmets and protective gear when driving or playing sports; Always wear your seat belt while in a vehicle; Limit alcohol consumption as much as possible.

Không uống rượu bia khi lái xe
Acute epidural hematoma needs to be noticed and treated promptly when there are signs and symptoms. Because prevention is always better than cure, it is necessary to take measures to protect yourself from the smallest things to avoid causing unfortunate consequences.
MORE:
How dangerous is a subdural hematoma after an injury? Chronic subdural hematoma in the elderly Subdural hematoma: Symptoms, diagnosis and treatment