This is an automatically translated article.
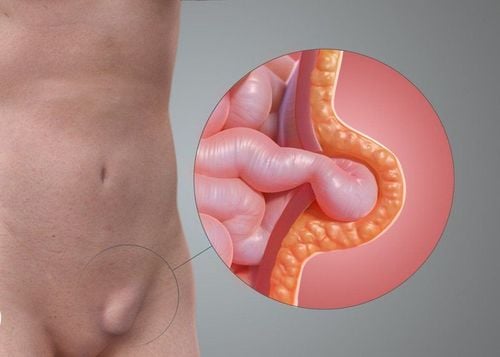
Inguinal hernia is a phenomenon in which the viscera inside the peritoneal cavity come out through a weak point in the posterior wall of the inguinal canal. The disease often causes discomfort, affects daily life as well as work, sometimes also endangers the patient's life. Inguinal hernia is treated by surgical methods such as surgery to remove only the hernia sac, surgery to remove the hernia sac with restoration of the abdominal wall behind the inguinal canal,...
1. Inguinal hernia surgery methods and principles
1.1 Surgical methods of inguinal hernia
Surgery to treat inguinal hernia is divided into 3 types:
Herniotomy: Surgery to remove only the inguinal hernia sac. Herniorrhaphy: Surgical removal of the hernia sac with restoration of the abdominal wall behind the inguinal canal. Hernioplasty: Surgical removal of the hernia sac with restoration of the abdominal wall behind the inguinal canal with an artificial mesh.
1.2 Principles of inguinal hernia surgery
There are two main steps in the surgical treatment of inguinal hernia, which is the treatment of the hernia sac and the restoration of the inguinal floor. The principle of handling the hernia sac is to separate the spermatic cord from the inguinal floor, separate the inguinal hernia sac from the spermatic cord, followed by clamping across the neck of the bag and suturing the proximal end, then pushing the proximal end back into the abdominal cavity. . If the hernia sac is large, it is possible to leave the bag, but it is necessary to treat the neck of the bag as above. If the inguinal hernia sac has a wide neck, also known as a direct inguinal hernia, it is easier to turn the bag back into the abdominal cavity than to remove the bag.
Inguinal floor restoration has two main ways including:
Classical inguinal floor restoration: using the patient's own tissue to restore. Restoration of the inguinal floor "tension-free": using grafts to restore, is the trend of inguinal hernia treatment today. Surgery using the method of restoring the inguinal floor without tension has the advantages of less postoperative pain and low recurrence rate. Inguinal hernia surgery can be performed in two directions including anterior and posterior recline. Surgical methods for posterior inguinal hernia can be performed by open surgery or laparoscopic surgery.
Phẫu thuật thoát vị bẹn bằng phương pháp Bassinia
2. Lichtenstein surgery
Lichtenstein surgery is an open surgery technique belonging to the Hernioplasty group (removal of the inguinal hernia sac with reconstruction of the posterior adnexal wall by artificial mesh), currently considered the standard surgery in the treatment of inguinal hernia. Lichtenstein inguinal hernia surgery was performed for the first time by Lichtenstein. Today, however, this technique is much different from the technique presented by Lichtenstein. Lichtenstein surgery is most commonly used in the treatment of inguinal hernia, including the following steps:
Incision of the skin at the position above the medial 1/3 inguinal ligament. Open the superficial fascia, including the superficial Camper fat layer and the Scarpa fascia to the fascia of the external oblique muscle, and observe the external inguinal ring close to the upper third of the inguinal ligament. Open the deep fascia of the thigh and expose the femoral canal to examine for an accompanying femoral hernia. Open the fascia of the external oblique muscle at the position of the superficial inguinal ring about 5cm outward, taking care not to damage the inguinal iliac nerve. Dissect up and down behind the fascia of the external oblique muscle so that the underlying structures can be clearly seen, taking care not to damage the hypogastric nerve. Mobilization of the spermatic cord combined with the scrotal levator muscle, the iliac inguinal nerve and the femoral genitourinary nerve, the vascular bundle of the spermatic cord; All these structures are surrounded by a band of ice. Identify and isolate the hernia sac (located within the spermatic cord for indirect inguinal hernia and outside the spermatic cord for direct inguinal hernia). Tie and remove the hernia sac close to the deep inguinal ring. Place and fix the mesh (Mesh) in weak positions of the posterior wall of the inguinal canal. Thus, the graft is considered as a "new inguinal floor" and the place where the spermatic cord passes through the graft is considered as the "new deep inguinal". Remove the damaged nerve. In men, care should be taken to return the testicle to its normal position in the scrotum before closing the incision. Close the spermatic cord, external oblique fascia, subcutaneous tissue layer and skin.
3. Marcy surgery
Marcy's surgery is the simplest surgery to restore the inguinal floor and is often indicated in the case of a first degree inguinal hernia according to the Nyhus classification. The main content of marcy surgery is suturing deep inguinal stricture. The suturing of the deep inguinal stricture is performed by suturing (1-2 stitches) the transverse fascia to the pubic iliac band.
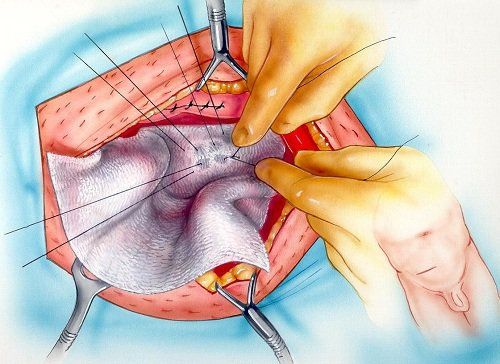
4. Bassini surgery
Inguinal hernia surgery by Bassinia method is the most classic surgery in the treatment of inguinal hernia and was most commonly performed before graft operations.
Techniques to perform bassini surgery include:
Incision to open the transverse fascia from the deep inguinal ring to the pubic tubercle to expose the underlying preperitoneal fat. Suture the inguinal ligament (Poupart's ligament) to the transverse fascia, the transverse fascia, and the internal oblique muscle (triple suture), starting at the pubic tubercle (avoid suture to the periosteum as this may lead to osteomyelitis). later) to the deep inguinal ring.
Phẫu thuật thoát vị bẹn bằng phương pháp Bassinia là phẫu thuật kinh điển nhất
5. Shouldice surgery
Shouldice surgery is said to be the classic surgery with the lowest recurrence rate in the treatment of inguinal hernia. Techniques for performing shouldice surgery include:
The inguinal floor is improved by four layers and continuous stitches. The innermost layer starts from the pubic tubercle to the deep inguinal ring: suture the pubic iliac band with the posterior surface of the rectus abdominis posterior capsule internally, the inferior surface of the transverse fascia-transverse muscle-internal oblique fascia on the outside. In the second layer, from the deep inguinal ring to the pubic tubercle: suture the inguinal ligament to the lower border of the internal transverse oblique muscle fascia. Third and fourth layers: suture the medial transverse-oblique muscle to the medial surface of the flap below the external oblique muscle, parallel to and just above the inguinal ligament, creating two “artificial” inguinal ligaments.
6. Surgical restoration of the inguinal floor with a iliac band
The pubic iliac band is considered by Condon to be a structure that plays a key role in the surgical restoration of the inguinal floor. Surgical restoration of the inguinal floor with a iliac band by suturing the inguinal crescent to the transverse fascia-transverse muscle-internal oblique muscle, with separate sutures.
MORE: Can an inguinal hernia recur after surgery?
7. Inguinal floor rehabilitation by Mcvay's surgery
Surgery to restore the inguinal floor by Mcvay surgery is the classic surgery of choice for cases of direct inguinal hernia, indirect inguinal hernia with large hernia sac, femoral hernia and recurrent inguinal hernia .
Surgical techniques to restore the inguinal floor by the Mcvay method include:
Restoration of the inguinal floor by suturing the transverse fascia - transverse fascia - internal oblique muscle with Cooper's ligament, with separate sutures. The last stitch on the Cooper's ligament on the medial side of the femoral vein is called a transition stitch. Transitional suture with additional femoral sheath. The transition stitch has two effects: it narrows the femoral ring and creates a “smooth transition” between the Cooper and inguinal ligament stitches. After the transition stitch, the next stitches are the same as in Bassini surgery. Usually the surgeon will make an additional incision for decompression.
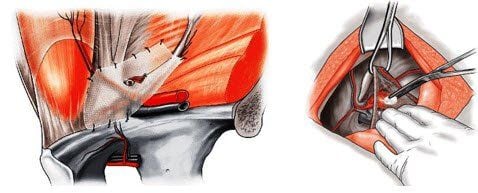
8. Reclining surgery
Reclining surgery is indicated in cases of inguinal hernia where the anterior wall has lost its normal anatomical structure or has recurred, or it is necessary to treat herniated organs such as strangulated hernia, hernia. slippage and femoral hernia. Retrograde surgery in the treatment of inguinal hernia is believed not to damage the sensory nerves of the inguinal region (because it does not require dissection of the spermatic cord).
The most important thing when performing retrograde surgery is that the surgeon must master the anatomical structure behind the inguinal wall. Posterior reclining surgery techniques include:
The posterior recline surgery is performed through a transverse incision on the lower abdomen and on the inguinal position about 2 cm deep. After removing the fascia of the anterior abdominal wall, the surgeon will enter the preperitoneal space. If the hernia is bilateral, it is possible to enter the preperitoneal space through a midline incision below the umbilicus. The hernia sac is treated before the inguinal floor is restored. The inguinal floor can be restored classically, by suturing the transverse fascia and transverse fascia with the pubic iliac band and Cooper's ligament, and can also be restored by graft placement. After suturing the inguinal floor by classical methods, grafts can be placed to further strengthen the inguinal floor. It should be noted that the suturing of the graft must be done very carefully, to avoid damage to important blood vessels and nerves. Just 2-3 stitches are enough to keep the graft in place. Whether the graft is dissected to allow passage of the testicular vessels and vas deferens. If the graft is not dissected, the vas deferens and testicular vasculature must be formed.)

Phẫu thuật thoát vị bẹn bằng phương pháp phẫu thuật ngả sau
9. Laparoscopic inguinal hernia surgery
9.1 Laparoscopic surgery through the abdomen into the preperitoneal space
Laparoscopic surgery through the abdomen into the preperitoneal cavity by:
Placement of trocars: 10mm magnoscope trocar placed at the navel penetrates into the abdomen, 2 5mm trocars placed on both sides of the rectus muscle, away from the navel line 4-5cm below. If a clip is used to fix the mesh, the right trocar should use a 10mm trocar. Laparoscope (Optic): use tilt type 300 or glass type 00. To enter the inguinal area, it is necessary to conduct peritoneal opening. The peritoneal opening started from the medial umbilical ligament and then to the anterior superior iliac spine, about 2 cm above the hernia opening. The lower peritoneal fold is widely exposed to the entire foramen commissure, deep inguinal ring, pubic bone, and pubic band. Dissection of the hernia sac: the direct hernia sac is pulled inward, the indirect hernia sac must be dissected from the spermatic cord. Tie the hernia sac with undissolved thread, then cut the sac near the deep inguinal ring. Placement of the mesh: the polypropylene mesh is rolled up and inserted into the abdomen through the trocar microscope, completely covering the foramen sphincter inserted into the spermatic cord. Fixing the mesh: Small sized meshes should be fixed. The peritoneum is closed after the mesh is placed.
9.2 Complete laparoscopic extraperitoneal surgery
Location of trocars in laparoscopic completely extraperitoneal surgery: The most commonly used laparoscopic trocar is a 10mm trocar placed 1cm below the umbilicus and behind the muscle, in front of the posterior fascia of the rectus abdominis muscle on the same side as the hernia. Two 5mm surgical trocars, which can be placed in 3 ways: First: the first surgical trocar is placed between the pubic and navel, the second surgical trocar is placed at the superior border of the pubic bone (3 trocars are located on one side). straight line). The second method: a surgical trocar is placed between the pubic and navel, the second surgical trocar is placed in the iliac fossa opposite the side of the hernia. The third way: 2 surgical trocars combined with the bronchoscope trocar form an equilateral triangle. A CO2 pump with a pressure of 12 mmHg was used to dissect the extraperitoneal space, creating space for surgical trocar placement and exposing the hernia sac (Figure 8). Dissecting reveals the hernia sac: after the peritoneum is separated from the anterior and posterior abdominal wall, the hernia sac is most clearly revealed. Handling of hernia sac: for direct inguinal hernia: very simple treatment by pulling the hernia out of the hernia pit at the position of Hesselbach's triangle and pushing it back into the abdomen. For indirect inguinal hernia: If the hernia sac is small, dissect, remove, and then lower the peritoneal folds out of the vascular bundle, the external iliac bundle, and the posterior abdominal wall. Large hernia sac requires dissection of the hernia sac from the spermatic cord, tying the bag at high height, using non-dissolving thread, and cutting the bag right at the position of the deep inguinal ring, leaving the distal end open. The lower peritoneal folds are separated from the testicular vessels, vas deferens, external iliac vessels, and posterior abdominal wall. Expose the extraperitoneal space large enough to place the mesh so that the mesh is wide enough to cover the entire foramen without flexion. Surgical removal of fatty tumors outside the peritoneum, around the deep inguinal ring. Notice the size of the hernia: < 1.5 cm, from 1.5 to 3 cm and > 3 cm. Place a mesh panel that completely covers the foramen magnum and overlap the spermatic cord. Fixed or not fixed: large grafts do not need to be fixed. Release the CO2 slowly so that the peritoneum presses against the newly flattened mesh. In short, an inguinal hernia is a condition in which the internal organs of the peritoneal cavity come out through a weak point in the posterior wall of the inguinal canal. The disease often causes discomfort, affects daily life as well as work, sometimes also endangers the patient's life. There are many surgical methods to treat inguinal hernias such as surgery to remove only the hernia sac, surgery to remove the hernia sac with restoration of the abdominal wall behind the inguinal canal,... Each patient will have a choice of treatment method. Treatment varies depending on the medical condition of each person. Therefore, in order to ensure safety and limit complications after surgery for inguinal hernia, patients need to go to a medical facility for screening examination and appropriate treatment for inguinal hernia.
At the Department of General Surgery - Vinmec International General Hospital is applying robotic surgery in the treatment of inguinal hernia. The technique is performed by a team of highly experienced, experienced doctors, technicians and medical experts with the support of the world's leading modern equipment.
Inguinal hernia surgery at Vinmec uses Da Vinci robot - which converts the surgeon's movements into machine movements through computer communication between the system working directly on the remote patient and the table doctor control.
Hand-held robots have more flexibility than conventional endoscopes. The robot is attached with a motor and control unit to the endoscopic handle, which helps the surgical head function as a flexible wrist joint that can be angled. In addition, the instrument also includes an endoscope that automates through voice, laser, eye tracking and other methods, allowing the surgeon to control the laparoscope without an assistant holding the lamp when surgery.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.