This is an automatically translated article.
The article was professionally consulted by BSCK I Nguyen Xuan Tinh - Anesthesiologist - Resuscitation - Department of General Surgery - Vinmec Phu Quoc International General Hospital.Ectopic pregnancy is a disease encountered in obstetrics that can cause many dangerous complications for pregnant women. When an ectopic pregnancy ruptures, it needs to be treated surgically quickly to avoid the risk of affecting the patient's life. Endotracheal anesthesia is an anesthetic method used in surgery for ruptured ectopic pregnancy.
1. Endotracheal anesthesia in ectopic pregnancy surgery
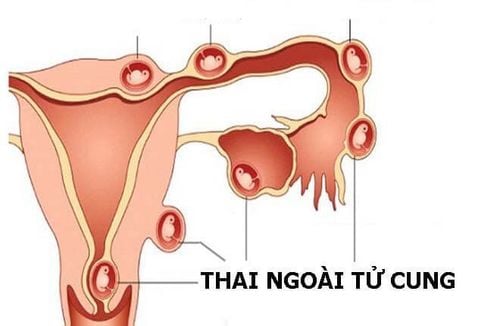
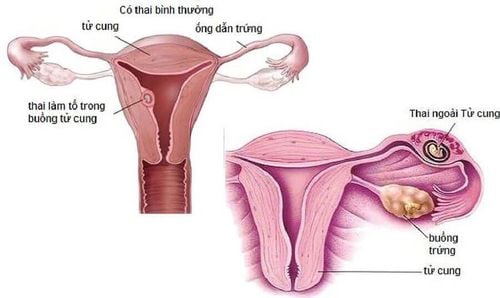
An ectopic pregnancy is when a fertilized egg implants outside the uterus. Ectopic pregnancy is common mainly in the fallopian tubes, in addition to the ovaries, cervix and abdominal cavity. As the fetus grows, it will cause compression and then rupture, leading to intra-abdominal bleeding, which can be fatal for pregnant women. This condition is called a ruptured ectopic pregnancy.For broken ectopic pregnancy, the treatment is urgent, treat as soon as possible to avoid affecting the health and life of the pregnant woman. In cases of ruptured ectopic pregnancy, the safest and most optimal treatment method is surgery. It is necessary to conduct surgery soon, to avoid the risk of shock and loss of blood affecting the life of the mother. . Endotracheal anesthesia in surgery for ruptured ectopic pregnancy is a general anesthetic technique that means the patient will sleep during the surgery with the aim of controlling breathing during surgery and resuscitation after surgery. art.
2. Endotracheal anesthesia technique in surgery for ruptured ectopic pregnancy
2.1 Indications and contraindications Indications:
Surgery is indicated in patients with ruptured ectopic pregnancy. If the fetus is bleeding recently, laparoscopic surgery can be used, however, in the majority of fetuses that have ruptured, open caesarean section is usually used. In surgery, but mask control is difficult. Use for maintenance of anesthesia with inhalation anesthetics. Contraindications:
Patient or family members disagree. Insufficient facilities and not proficient in endotracheal anesthesia techniques.

2.2 Procedure for endotracheal anesthesia Preparation
To perform endotracheal anesthesia requires a team of doctors and nurses specialized in anesthesiology.
Facilities:
Required equipment: Anesthesia machine system with ventilator; hand squeeze oxygen source; monitor vital functions such as electrocardiogram, arterial blood pressure, SpO2, EtCO2, breathing rate, temperature; defibrillator, phlegm aspirator. Laryngoscope, endotracheal tube of different sizes, suction tube, mask, bulb, oropharyngeal cannula, Magill pliers, soft mandrin. Drugs: Used in anesthesia resuscitation and treatment of accidents. Prophylaxis in case of difficult intubation: Cook tube, laryngeal mask, flexible bronchoscope, tracheostomy kit, mouth opener... Patient:
Full anesthetic examination before surgery , detect and prevent the risk of accidents that may occur. Advise and explain the possible complications of endotracheal anesthesia and surgery. Evaluation of cases at risk of difficult intubation. Use sedation the night before surgery if the patient is too nervous. Patients should be examined and pre-prepared for red blood cells to prevent the risk of serious, life-threatening bleeding. Procedure
Patient:
Patient position: Lie on back, breathe 100% oxygen 3-6 l/min at least 5 minutes before induction of anesthesia. Install a monitor to monitor vital signs, if laparoscopic surgery must have EtCO2 parameters. Establish an effective line and a line is required to prepare for transfusion. Pre-anesthesia: Fentanyl 100mcg and midazolam 2mcg Induction:
Anesthesia can be initiated by intravenous anesthetic (propofol, etomidate, thiopental, ketamine...), inhalation or a combination. Combine some drugs to increase the effect of anesthetics such as: opioid pain relievers (fentanyl, morphine...), muscle relaxants if necessary. Prophylaxis with H2-receptor antagonists and metoclopramide. Oral intubation: The condition for intubation is when the patient is in deep sleep, with enough muscle relaxation in most cases.
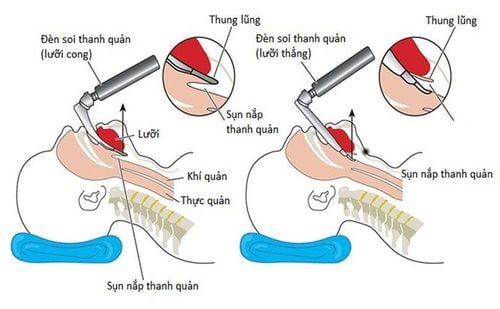
Open the patient's mouth, put one hand under the neck to help straighten the neck, put the laryngoscope to the right of the mouth, push the patient's tongue to the left, push the light deeply, coordinate with the right hand to press the cricoid cartilage, then find the lid glottis and glottis. Perform rapid induction of anesthesia and the Sellick maneuver in cases where the patient has a full stomach. Pass the endotracheal tube gently through the glottis, stopping when the balloon of the endotracheal tube passes about 2-3 cm across the vocal cords.

Remove the laryngoscope and inflate the endotracheal balloon. Check the correct position of the endotracheal tube with auscultation and EtCO2 results Secure the tube with tape and place the cannula in the mouth to avoid biting the tube (if necessary). In the case of difficult intubation, the difficult intubation procedure is applied. Maintenance of anesthesia: Maintain anesthesia with intravenous or inhalation anesthetics, combined with analgesia and muscle relaxants (if necessary).
Monitor:
Need to control breathing with ventilator or squeeze balloon. Monitor the depth of anesthesia based on heart rate, blood pressure, sweating, tearing... Preventing cases of endotracheal intubation in the wrong position, folding, or obstruction. 2.3 Criteria for extubation When the surgery is completed, the endotracheal tube should be extubated when the following criteria are met:
The patient is awake and follows orders; Lift head for more than 5 seconds, TOF >0.9 (if any); Spontaneous breathing, breathing rate within normal limits; Pulse, arterial blood pressure stable; Body temperature > 35 degrees Celsius; There are no complications of anesthesia and surgery.
3. Complications and management of complications due to intubation
3.1 Reflux of gastric juice into airway Signs: There is presence of digestive juices in the oral cavity and airways. Treatment: Drain the fluid, put the patient's head down, tilt the head to the side; Place the endotracheal tube quickly and clear the airway. Monitoring and prevention of lung infections after surgery. 3.2 Hemodynamic disorders Hemodynamic conditions may occur such as: hypotension or hypertension, cardiac arrhythmias (bradycardia, tachycardia, arrhythmia). Depending on each sign to take measures.
3.3 Complications due to intubation Failure to intubate: Treatment according to the procedure of intubation is difficult or if intubation is not possible, it is necessary to switch to another anesthesia method. Misplaced in the stomach: Signs: Auscultation of the lungs without alveolar murmurs, no measurement of EtCO2. Treatment: Reinsert the endotracheal tube. Vocal, air, bronchospasm Difficult or impossible pulmonary ventilation, auscultation with crackles or muted lung Management: Provide adequate oxygen, add hypnotics and muscle relaxants, ensure ventilation and give bronchodilators administration and corticosteroids; If breathing is not controlled, a difficult endotracheal intubation procedure should be used. Trauma when inserting the tube: Bleeding, broken teeth, damage to the vocal cords, falling foreign objects into the airways... Injury treatment depends on each case. 3.4 Respiratory complications Folding, retracting, causing the endotracheal tube to push deep into one lung, collapse or open the respiratory system, the oxygen source is exhausted...
Treatment: Need to ensure ventilation and provide 100% oxygen , find and solve the cause.

3.5 Complications after extubation Some complications after extubation can be encountered such as: respiratory failure, sore throat hoarseness, spasm of the larynx, trachea and bronchi, inflammation of the upper respiratory tract and narrowing of the larynx and trachea.
Treatment depends on each case and each cause.
3.6 Some complications after surgery Postoperative bleeding: in the first 6 hours, pulse, blood pressure and general condition must be monitored in the recovery room. If the pulse is rapid, the blood pressure is reduced, the abdomen is percussive, and the ultrasound has a lot of free fluid, it must be thought of internal bleeding, possibly due to the removal of the sutures in the area of the salpingectomy. Immediate surgery is required to stop the bleeding. Infection: During surgery, it is necessary to wipe off all the blood and blood clots in the abdomen to avoid infection. However, avoid wiping too carefully to cause abdominal adhesions because the serosa is damaged. Therapeutic doses of systemic antibiotics must be given to prevent infection, especially during blood transfusion. Endotracheal anesthesia is a technique that requires expertise and experience to avoid the risk of a number of complications. In case of ruptured ectopic pregnancy, it is necessary to conduct prompt treatment, helping to solve the blood loss to preserve the life of the pregnant woman.
Vinmec International General Hospital is one of the hospitals that strictly applies safe surgical anesthesia practice standards according to international guidelines. Vinmec has a team of experienced anesthesiologists and nurses, modern equipment such as: nerve detectors, ultrasound machines, Karl Storz's difficult airway control system, comprehensive anesthesia monitoring system GE's AoA (Adequate of Anesthesia) including monitoring of anesthesia, pain and muscle relaxation will provide high quality and safety, helping patients to have adequate anesthesia, not wake up, and do not have residual muscle relaxants after surgery.
Vinmec Health System is also proud to be the first hospital in Vietnam to sign with the World Anesthesiology Association (WFSA) towards the goal of becoming the safest hospital for surgical anesthesia in Southeast Asia.
Doctor Nguyen Xuan Tinh has more than 18 years of experience studying and working in the field of Anesthesia - Resuscitation. Before working as an anesthesiologist at the Department of General Surgery - Vinmec Phu Quoc International General Hospital, Dr. Tinh worked for a long time at Cam Xuyen Tinh District General Hospital, Ha Tinh.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.