This is an automatically translated article.
Post by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
The sphincter of Oddi is a smooth muscle valve that regulates the flow of bile and pancreas into the duodenum, first described by the Italian anatomist, Ruggero Oddi, in 1887. Sphincter of Oddi dysfunction (sphincter of Oddi) D) is a broad term used to refer to a variety of biliary, pancreatic, and liver disorders caused by constriction, tightening, and dilation of these valves at inappropriate times.
1. Overview
This review addresses various factors that may increase the risk of a ring of Oddi D, including but not limited to: cholecystectomy, drug and alcohol use. Lack of recognition and appropriate treatment of the sphincter of Oddi D may be associated with clinical events, including pancreatitis and biliary symptoms associated with elevated liver enzymes. Pharmacologic and non-pharmacological approaches are discussed to help recognize, prevent, and treat the sphincter of Oddi D. Future studies are needed to evaluate the therapeutic benefit of drugs such as drugs. calcium channel blockers, glyceryl trinitrate, or tricyclic antidepressants in patients with the sphincter of Oddi D.
2. Structure and function of the sphincter of Oddi
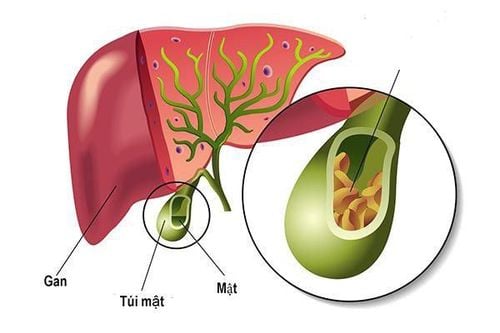
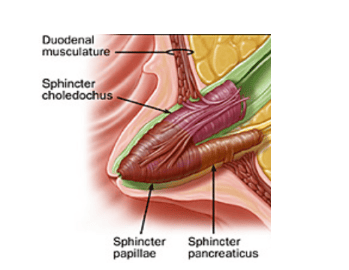
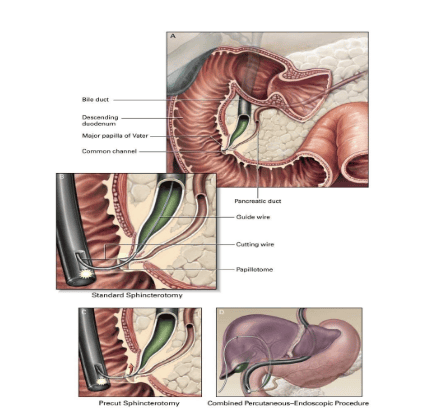
The sphincter of Oddi is a muscular structure that surrounds the confluence of the distal common bile duct (common bile duct) and pancreatic duct (pancreatic duct) into the duct of Vater. The structure of the sphincter of Oddi with the upper mucosa protruding into the duodenum is called the Vater papilla. At least three functions of the sphincter of Oddi have been identified: (1) regulation of bile flow into the duodenum; (2) prevention of duodenal reflux; and (3) regulation of gallbladder filling by bile displacement into the gallbladder with closure of the sphincter of Oddi .
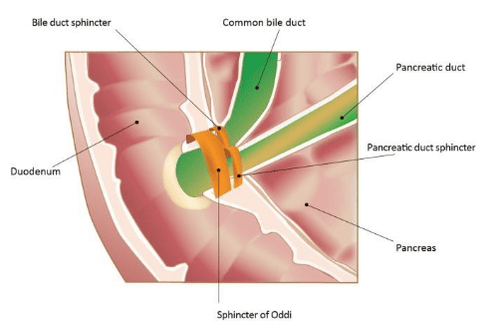
Sphincter of Oddi (sphincter of Oddi) and its anatomical relationships. In the majority of patients, pancreatic juice and bile enter the duodenum through the sphincter of Oddi. The sphincter structure with the upper mucosa protruding into the duodenum is called the Vater papilla. In addition, there are individual sphincters for both the common bile duct and the pancreatic duct near the sphincter of Oddi. All sphincters are controlled by nerves.
3. Physiology of the sphincter of Oddi
The physiology of the sphincter of Oddi has been studied in both animals and humans. While different species have been studied, the physiology of dogs, cats, and pigs closely resembles that of humans. It is important to consider the species studied when analyzing pharmacological data. In humans, the basal pressure of the sphincter of Oddi is 10 mmHg. The superimposed antagonistic phagocytic contractions, beginning at the junction of the common bile duct and the sphincter of Oddi and entering the duodenum, occur in response to physiological and exogenous stimuli and lead to migration. substances already present in the sphincter of Oddi into the duodenum. During contraction, no additional flow from the common bile duct into the sphincter of Oddi occurs. The sphincter of Oddi then relaxes, allowing passive intake of bile into the sphincter of Oddi segment. Once filled, another wave of phasic contractions begins. As basal pressure increases, resistance to flow increases, leading to gallbladder filling and obstruction of duodenal outflow. When the basal pressure falls below the common bile duct and pancreatic duct pressure, duodenal outflow occurs.
Peristaltic patterns of the sphincter of Oddi have been identified for both the gastrointestinal and gastrointestinal tracts. During the mid-digestive phase, the sphincter of Oddi has a cyclical pattern of activity during all phases and increases in frequency before phase 3 of duodenal activity, promoting bile secretion and pancreas into the duodenum. Mobility during digestion involves both neural and hormonal inputs. This period has gallbladder contractions, stimulates the pancreas to secrete fluid, relaxes the sphincter of Oddi, leading to an increased ratio of bile and pancreatic juice to the duodenum. It should be noted that, in the digestive phase, there are different phases of the meal, each of which provides input. For example, up to 30–40% of gallbladder emptying and 25% of pancreatic secretion occur in the cyclic phase via vagal input, while another 10–20% occur during the cyclic phase. gastric passage through the vagovagal pathway. However, the gallbladder excretes most of its remainder, and the pancreas, up to 50% of its total excretion, in the intestinal phase, produced by the release of cholecystokinin (CCK) and secrettin from the duodenum and proximal jejunum. Duodenal CCK contracts the gallbladder, relaxes the sphincter of Oddi, and induces pancreatic exocrine digestive enzyme secretion through direct action on CCK receptors and indirectly via cholinergic neurons. This is supported by the observation that atropine pretreatment suppresses gallbladder contraction and pancreatic secretion due to physiological concentrations of CCK and by a high-protein meal.
4. Hormones and neurotransmitters involved in the function of the sphincter of Oddi
The most important hormone involved in sphincter of Oddi function is CCK. CCK released from enterocytes in response to a meal has a direct hormonal effect as well as an indirect effect by interacting with neural pathways, resulting in gallbladder contraction and glandular enzyme secretion. pancreas. CCK reduces the basal sphincter of Oddi pressure and inhibits phasic contractions, thereby promoting retrograde flow. Intestinal active polypeptides and nitric oxide, present in the intrinsic neurons of the sphincter of Oddi, have been implicated in the relaxation response to CCK as well as the relaxation observed during the happy phase of the sphincter. meal.
Motilin, somatostatin and octreotide affect sphincter of Oddi function. Motilin, secreted by M cells in the duodenum and jejunum, causes contraction of the smooth muscle of the gallbladder and stimulates bile secretion. Somatostatin, present in endocrine cells throughout the gastrointestinal tract, has the potential to exert an inhibitory effect on both gallbladder contractility and sphincter of Oddi relaxation, which is supported by the observation that 50 μg of octreotide administered intravenously , a somatostatin mimetic agent, increases the sphincter of Oddi basal pressure and frequency of contractions.
5. What is sphincter of Oddi dysfunction?
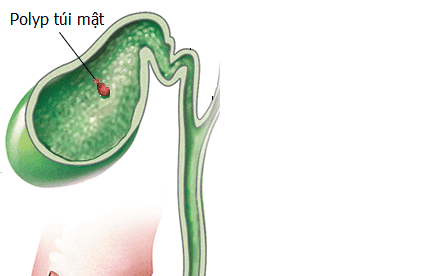
Sphincter of Oddi dysfunction is a clinical syndrome caused by dyskinesia of the sphincter of Oddi (functional) or anatomical (mechanical) obstruction associated with abdominal pain and elevation of liver or pancreatic enzymes, ductal dilation. common bile or pancreatic duct, or pancreatitis. Note that the term sphincter of Oddi dyskinesias more specifically denotes dyskinesias of the sphincter of Oddi, while the sphincter of Oddi includes both mechanical obstruction and dyskinesia of the sphincter of Oddi. In this context, the term biliary dyskinesia has historically been used as a generic term to include both sphincter of Oddi dyskinesia and gallbladder dyskinesia. Various forms of primary sphincter of Oddi are considered functional gastrointestinal disorders and can occur in adults or children of any age, but sphincter of Oddi disorder is most common in women aged 20– 50 years old.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.