This is an automatically translated article.
Being infected with HP bacteria is a very common condition nowadays. After treatment, many people still wonder with the question of HP bacteria recur? The following article will help readers answer this question.
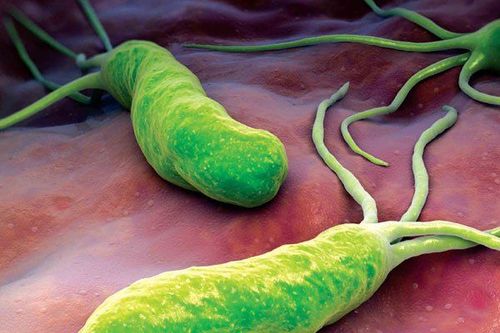
1. What is Helicobacter pylori?
Helicobacter pylori was first discovered in 1982. This is a spiral-shaped bacteria, usually found in the stomach of infected people. Most people with H. pylori in the stomach have no symptoms and don't have any health problems. However, HP bacteria are also capable of causing a number of gastrointestinal diseases (including peptic ulcers, and rarely, stomach cancer).
When infected with HP, most patients do not have any symptoms. However, when the infection causes an ulcer in the stomach or duodenum, the patient may experience a number of symptoms such as: Pain or discomfort in the upper abdomen, swelling or bloating, feeling full even when eating little food, boredom eating, nausea or vomiting, dark or tarry stools, bleeding sores causing anemia and fatigue,...
Regarding treatment, if infected with HP bacteria but do not have any problems problem and infected people who are not in a high-risk group for stomach cancer may not need treatment. However, in patients with a history of peptic ulcer, active gastric ulcer, or duodenal ulcer associated with HP infection, treatment is necessary. Successful treatment of HP helps ulcers heal faster, prevents ulcers from recurring, and reduces the risk of complications such as bleeding. In addition, patients who are taking long-term anti-inflammatory drugs such as Aspirin, Ibuprofen, Naproxen or similar drugs to treat arthritis should be tested for HP, if infected must be treated to destroy HP.
2. Does the HP virus recur?
According to doctors, HP bacteria are easy to recur. It is a worrying fact that even though a patient has been diagnosed with HP infection and successfully undergoes eradication, the patient is still at risk of reinfection.
According to statistics, in Vietnam, on average 11 months after completely eradicating HP, HP bacteria reappeared in the stomach with the rate of 23.5%. In which, the rate of re-infection (completely cured but then re-infected) was 9.7%, the rate of recurrence was 13.8%. In contrast to our country, the rate of HP re-infection in the stomach in developed countries such as the US, Japan and Finland is very low, only about 0.2 - 2%.
Recently, a study also proved: Even if HP treatment is completely gone, on average after about 1 year, the rate of re-infection still accounts for about 10%.
Reinfection with HP can increase the risk of recurrent gastric disease by 4 times, and also increase the complication rate of peptic ulcer by 15-20%. Therefore, patients should find appropriate measures to treat HP thoroughly.
3. Causes of HP . bacteria recurrence
After being infected with HP bacteria and treated, the patient can still have a recurrence of HP infection if they do not follow the treatment regimen, have an inappropriate diet, and come into contact with medical equipment. In which, there are 2 main causes of gastric HP bacteria recurrence, including:
3.1 HP is a highly infectious and re-infective bacteria strain HP can infect, re-infection through many ways such as:
Oral - Oral: This is the most common way of HP infection. Because HP bacteria exist in the patient's saliva, oral cavity, teeth, ... so when we kiss, share dishes, ..., this bacteria can spread easily; Stomach - mouth: HP bacteria cause stomach ulcers, causing patients to have acid reflux, heartburn, ... When the patient sneezes or breathes heavily, HP bacteria can spread to those in contact. close to the patient; Stool - mouth: In the stool that the patient excretes, there is a large amount of HP bacteria. After going to the toilet, if the sick person does not clean properly, it can cause HP bacteria to be spread when they handle food with their hands, touch other objects and surfaces,... In addition, the Intermediate animals such as mosquitoes, flies, cockroaches, mice, ... also contribute to the spread of HP bacteria through this route. Therefore, after successfully treating HP bacteria, if the patient is still exposed to infectious sources of this bacterium, there is a complete risk of re-infection.
3.2 HP bacteria may still exist from the previous treatment. When using anti-HP drugs, the bacteria have not been completely destroyed but only reduced in number, HP can no longer be detected in the stomach by other methods. testing method. However, the bacteria then multiply and recur. The reason is that because many patients are resistant to drugs, HP bacteria cannot be killed by conventional methods.
HP bacteria were previously very sensitive to antibiotics, so they were easily destroyed. In the years 1990 - 2000, the success rate of killing HP was very high. With only 2 of 2 antibiotics such as Amoxicillin, Clarithromycin and Metronidazol, the effectiveness of killing more than 95% was achieved with only 7 days of treatment.
However, up to now, antibiotic resistance in Vietnam is very high, on average: Amoxicillin 24.9%, Levofloxacin 27.9%, Clarithromycin 34.1% (85.5%) in research, Metronidazole 69.4% (95.5%), Tetracycline 17.9% and at the same time resistant to many antibiotics on average 47.4%. Thus, the treatment of HP becomes more difficult, it is necessary to have the right indication, only to destroy it when it is really necessary.
4. Measures to prevent the recurrence of gastric HP bacteria
To avoid the risk of gastric HP infection or recurrence, patients should note:
Go to a doctor and strictly follow the treatment regimen prescribed by the doctor. Currently, regimens to kill HP bacteria often combine multiple antibiotics to use for about 4-6 weeks. Patients should take serious treatment to completely eliminate this stubborn strain of bacteria, reducing the risk of recurrence later; Use drugs in the right dosage, right antibiotics prescribed by the doctor, absolutely do not buy drugs to use on their own; Should regularly check the disease status to have appropriate treatment; Develop the habit of washing hands thoroughly with soap before eating and after using the toilet to prevent the spread of bacteria; Do not use food that has not been thoroughly cooked or has signs of mold, infection or rancidity; Drink clean water, use clean water during food processing; Limit eating at stores that do not ensure food hygiene and safety; Eat cooked, drink boiling, avoid sharing eating utensils such as cups, bowls, chopsticks, spoons,...; Limit hand contact in places where HP bacteria often reside in prison such as stairs, dining tables,... Do not use saliva to turn paper, count money,...; Building a scientific and healthy eating menu; If someone in the family has duodenal and gastric duodenal disease due to HP infection, in parallel with HP treatment for the patient, it is necessary to check for HP infection for all family members to take measures to prevent re-infection. . When suspected of being infected with HP bacteria, the patient should go to the doctor soon for diagnosis and appropriate intervention advice. With all the instructions of the doctor, the patient needs 100% coordination to ensure good treatment effect, avoid the risk of re-infection with HP or dangerous diseases in the stomach.
Follow Vinmec International General Hospital website to get more health, nutrition and beauty information to protect the health of yourself and your loved ones in your family.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.