This is an automatically translated article.
Dr. Department of Gastroenterology - Endoscopy, Vinmec Central Park International General Hospital
1. GENERAL OBJECTIVES
Every year in the US there are 21,000 new cases. The frequency is down by a third compared to 40 years ago. This may be due to a reduced frequency of infection with Helicobacter pylori, a known cause of stomach cancer.
Helicobacter pylori is thought to cause chronic gastritis, which can lead to stomach cancer. This bacterial infection increases the incidence of cancers in the body and antrum (not in the cardia) by 3.6-18 times.
In the US there are 10 new cases for 100,000 people. The highest is in Costa Rica with 53 new cases per 100,000 population. In central and eastern Europe, the frequency is 35 cases per 100,000 people. Epidemiological surveys show that stomach cancer is associated with a low intake of vegetables and fruits. Stomach cancer rarely occurs under the age of 40, then increases gradually. The average age is 63 and men are twice as many as women.
Stomach cancer is usually adenocarcinoma. Squamous cell cancer is often associated with esophageal cancer. There are 5 pathological forms:
Ulcer type (25%): this is a deep ulcer, penetrating all layers of the stomach wall and can spread to adjacent organs. The margin of the ulcer is concave, unlike a benign ulcer with a raised edge. Polypoid form (25%). Superficial spreading cancer (15%): also known as early stage cancer, eats into the mucosa and submucosa of the stomach. Metastasis in 30% of cases. Even with metastases, after gastrectomy, the prognosis is better than advanced cancer. In Japan, the screening program shows that 30% are early stage cancers and survival time is significantly increased. Linitis platica (15%). Prognosis is poor because the cancer spreads quickly and early. Extensive cancer (35%): in this large group, the tumor is partly located in the lumen of the stomach and partly outside. Gastric adenocarcinoma is also classified according to the degree of cell differentiation. In general, the spread depends on the resolution. Some cancers that cause reactivity in neighboring cells have a good prognosis.
Intestinal type cancer has a better prognosis than diffuse type. The type of intestinal cell commonly found in Japan and Finland is where many stomach cancers are found. The reduction in the number of cancers in these countries is due to a decrease in the type of enterocytes. The signet cell type increased and now accounts for a third of cases. This type presents as invasive cancer in women and young adults and occurs in the distal stomach. Helicobacter pylori infection does not affect the type of cancer cells.
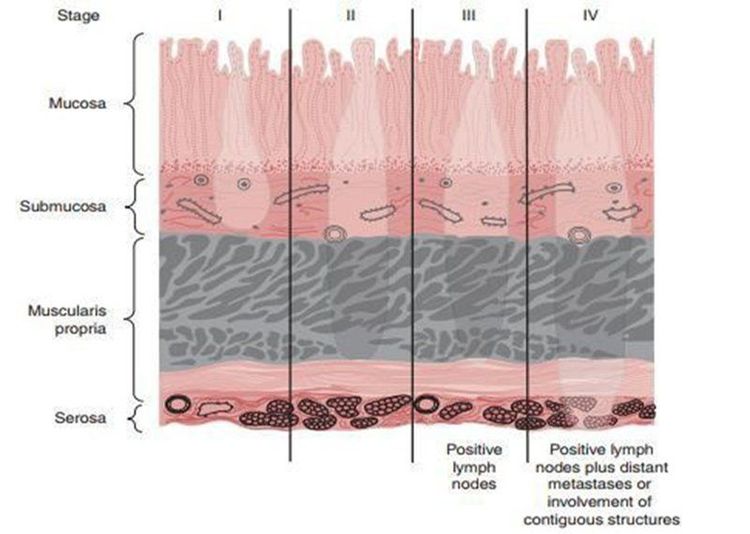
Spread occurs within the gastric wall, directly outside the stomach, and metastasizes by lymphatic vessels. Staging is closely related to survival time shown in Figure 1.
3 4 patients at diagnosis have metastasized . In the lumen of the stomach, the spread is more upward than downward. The pylorus serves as a partial barrier, but 25% of cancers are located in the first few centimeters of the duodenal bulb.
Early gastric cancer is defined as cancer located in the mucosa or submucosa, with or without lymph node metastasis, with a good prognosis (5 year 90% survival after tumor resection). In Japan, this type of screening accounts for 30% while in the US only 10%.
40% of cancers are located in the antrum, mainly the small curvature, 30% in the body and gastric aneurysm, 25% in the cardia and 5% in the whole stomach.
The location of the cancer also varies, more proximal to the stomach today than 10-20 years ago. Ulcers in the great curvature and the cardia to watch out for are cancerous.
I. CLINICAL
1.1. Symptoms Early symptoms are heaviness in the abdomen after eating, making the patient not feel pain. Sometimes this uncomfortable feeling lasts for years and then more.
Anorexia appears early and especially with meat. Weight loss, the most common symptom, is usually 5-6 kg. Postprandial pain is easily mistaken for an ulcer, especially if the patient has previously had an X-ray showing an ulcer. Vomiting may occur, most often when pyloric stenosis is present. The vomit is the color of coffee grounds due to a bleeding tumor. There may be choking if the cancer is in the cardia.
1⁄4 of cases when abdominal examination revealed epigastric tumor. 10% found to have an enlarged liver. 50% showed microscopic blood in the stool and a few cases showed black blood (melena). Also other symptoms are of metastatic cancer. Metastasis to the neck through the thoracic duct produces Troisier's lymph nodes, also known as Virchow's nodes. Rectal examination revealed a Blumer shelf, an anterior rectal metastasis. Metastasis in the peritoneum into the ovary is called a Krukenberg tumor. Other metastases include liver, lung, brain, and bone.
1.2. Subclinical 40% of patients have anemia. CEA (carcinoembryonic antigen) was found to be elevated in 65% of cases indicating progression of the disease.
1.3. Imaging Barium radiographs are diagnostic in many cases, but the false-negative rate is 20%. The big problem is ulcerative cancer because it is difficult to distinguish from benign ulcers. All new patients with peptic ulcers should undergo gastroscopy and biopsy.
1.4. Gastroscopy and biopsies Large endoscopic tumor is known immediately. Any lesion, whether ulcerative or polypoid, should be biopsied and combed during endoscopy. At least 6 samples should be biopsied to avoid errors.

II. TREATMENT
2,1. Endoscopic mucosal resection (EMR) Born in 1984, is applied to well-differentiated adenocarcinoma, the size is not more than 20mm, does not invade the muscle layer. Benefit is a minimally invasive procedure. The disadvantage for large cancers is that it is not possible to take the entire sample for accurate testing.
2.2. Endoscopic Submucosal Dissection (ESD) Can be applied to cut en-bloc superficial tumors of large size. Complications are bleeding and perforation. Perforation can clip the clip and usually does not require reoperation.
2.3. Surgery (Gastrectomy) Surgery is the most radical treatment. 85% of patients can still operate and 50% can remove the tumor. Of these, half are curative. The majority of patients received chemotherapy before surgery.
The principle of surgery is to remove the tumor and regional lymph nodes and, if necessary, remove additional adjacent organs. Need to cut on the hump 6 cm. If the tumor is in the antrum, then the distal gastrectomy with the great omentum, 3-4 cm duodenum, subpyloric lymph nodes, left gastric artery and associated nodes. Reconstruction will do Billroth I or II, but Billroth II should be preferred because the tumor may later recur and block the anastomosis of Billroth I.
Total gastrectomy with splenectomy applies to cancer of the proximal stomach or form of linitis platica. Should splenectomy or not is debatable. The gastrointestinal tract was reconstructed according to Roux-en-Y. Hunr-Lawrence bags are not beneficial and can cause early complications.
For heart cancer, surgery through 2 thoracic and abdominal incisions cuts the lower part of the esophagus plus the spleen. If available, a cold biopsy of the proximal anastomosis should be performed. If there are cancer cells in the test tissue, it must be cut more widely because the cancer can spread in the lining of the stomach.
Temporary resection is applied when the tumor is still mobile and the patient's life is more than 1-2 months. Temporary resection is usually to remove the tumor in the antrum to avoid strangulation. Total gastrectomy can also be performed if it is safe and the tumor has not spread beyond the stomach. If possible, temporary resection is still better than gastro-jejunostomy.

III. PROPOSAL
In the US the 5-year survival rate is 12%. The 5-year survival rate for early stomach cancer is 90%. Survival rate relative to stage:
Stage I: 70% Stage II: 30% Stage III: 10% Stage IV: 0%. Death is due to tumor spreading to other organs or gradual gastric obstruction and malnutrition.
CONCLUSION
Stomach cancer is a serious disease with poor prognosis because patients often go to the doctor late. EMR and ESD are new, less invasive procedures.
Distal gastrectomy and D2 lymph node dissection are standard surgery for antral cancer. The disease should be detected early when there are digestive disorders, weight loss, anorexia.
At Vinmec, gastric cancer screening is done through gastric endoscopy with NBI (Narrow Banding Imaging - endoscopy with narrow light band) for clearer mucosal pathological analysis results. compared with conventional endoscopy.
Besides, with the system of Laboratory Department - Vinmec International General Hospital is a synchronous testing center with a full range of fields: Biochemistry, Hematology - Blood Transfusion, Microbiology - Parasitology and Solution Pathology and 3 majors: Biochemistry, Hematology - Blood Transfusion, Microbiology - Parasitology all achieved ISO 15189:2012 certificates. Vinmec Institute of Stem Cell and Gene Technology also screened 15 common cancers in Men and 17 common cancers in Women with only one gene test.
If you have a need for consultation and examination at Vinmec Hospitals under the national health system, please book an appointment on the website for service.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
SEE ALSO:
Stomach cancer surgery with advanced endoscopic techniques Nutrition for stomach cancer patients When to screen for stomach cancer?