This is an automatically translated article.
The article was written by MSc Vu Duy Dung - Doctor of Neurology, Department of General Internal Medicine - Vinmec Times City International HospitalCancer patients may develop myelopathy as a side effect of cancer treatment (systemic chemotherapy, intramedullary chemotherapy, immunotherapy, or radiation therapy) immunocompromised survival, and myelopathy from physician-induced surgical causes. The following sections describe spinal cord disease caused by chemotherapy, immunotherapy, and radiation therapy.
Paraneoplastic neuropathies are not covered in this article.
1. Spinal cord disease secondary to chemotherapy Methotrexate and cytarabine (Ara-C) are indicated as intramedullary chemotherapy in the treatment and prevention of CNS dissemination in patients with leukemia. (leukemia). Rarely, non-leemic patients may develop myelopathy associated with either of these CSF therapies. Symptoms may appear days to months after intrathecal injection of methotrexate. MRI shows T2 abnormalities in the posterior spinal column resembling subacute combined degeneration of the spinal cord. Proposed mechanisms are neurotoxicity from local folate depletion due to methotrexate or aseptic meningitis secondary to preservative use during methotrexate preparation. Chemotherapy with Ara-C alone can also induce myelopathy, and the underlying mechanism for the occurrence of myelopathy is unclear, but an inflammatory response to chemotherapy in the CSF is thought to be an reason. A retrospective study of 120 patients with cerebrospinal cystic fibrosis treated with intramedullary or intraventricular Ara-C found that myelopathy, cauda equine syndrome, and encephalocytemic syndrome were present in 7 ,5% of patients.
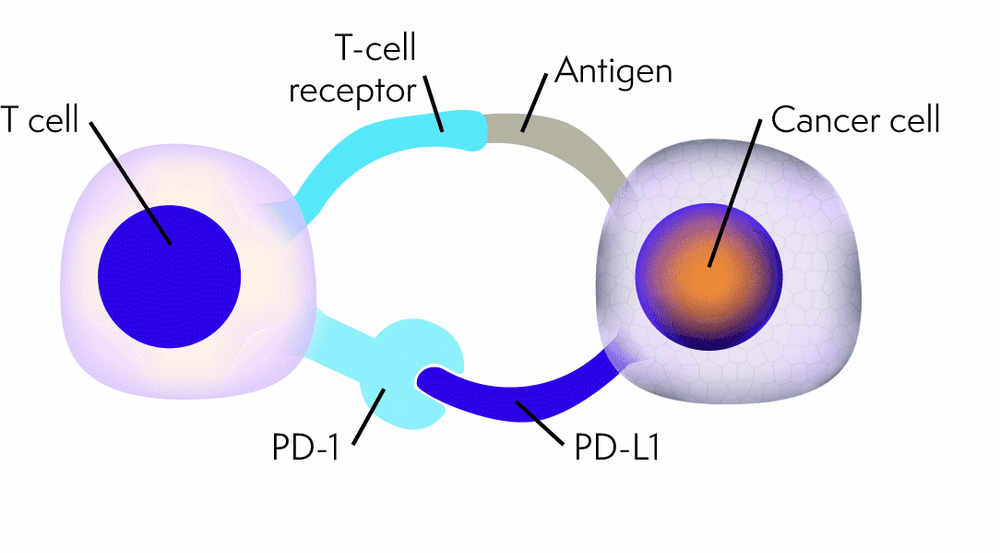
2. Spinal cord disease associated with immune checkpoint inhibitors Immunotherapy for cancer with immune checkpoint inhibitors is based on the understanding that tumor cells escape the system immunogenicity by dysregulating immune checkpoint pathways by overexpressing immunosuppressive surface ligands. Immune checkpoint inhibitors are monoclonal antibodies that bind to immune checkpoints such as cytotoxic T lymphocyte-associated protein 4 (CTLA-4), programmed death receptor 1 (PD1), and its ligand, PDL1. These immune checkpoint inhibitors act as inhibitory regulators of T-cell function. Currently, many immune checkpoint inhibitors such as nivolumab (ani-PD1), pembrolizumab (anti-PD1), ipilimumab (anti-CTLA-4) and durvalumab (anti-PDL1) are being studied for the treatment of melanoma. cancer, lung cancer, renal cell cancer, and central nervous system cancers.
3. Spinal cord disease associated with radiation therapy The spinal cord can be exposed to radiation when treating the spinal cord itself, the bones of the spine, the tissue around the spine, or the head, neck, and lung cancer. A routine 45 Gy to 50 Gy divided daily dose of 1.8 Gy to 2 Gy has a low risk of permanent myelopathy, estimated at 0.03% to 0.2%. However, when radiation-induced spinal cord disease is present, it can be a devastating complication.
Radiation toxicity to the spine can be divided into 3 categories: early injury, late but early injury, and late injury. Early damage occurs as a result of increased tumor edema and presents similar to the symptoms of epidural compression. Late but early damage occurs after a latent period of 2 to 4 months. The classic presentation of a late but early lesion is the Lhermitte sign characterized by electric shock or paresthesia sensations in the spine and extremities during neck flexion. Patients usually recover after a few months. Late radiotherapy damage to the spinal cord is usually irreversible, occurs more than 6 months after radiation therapy, and is classically referred to in the literature as radiation myelopathy. Radiation myelopathy is defined as an injury to the spinal cord caused by ionizing radiation due to destruction of white matter, blood vessels, and other nerve tissue after a certain latent period (usually 6 months). . On histopathology, white matter is often destroyed myelin and nerve fibers. Coagulation and liquid necrosis may be present. When white matter damage is severe, gray matter will be affected secondary. Vascular changes in the form of angiogenesis, vitreous degeneration, perivascular fibrosis, fibrinoid necrosis, and thrombosis have been observed. Symptoms are paresthesias and muscle weakness beginning in the legs.
Patients may experience circular muscle dysfunction, hemiplegia, gait ataxia, and paraplegia as the lesion progresses. Radiation myelopathy is considered a diagnosis of exclusion, and cancerous lesions of the spinal cord should be excluded. MRI shows low signal on T1, high signal on T2, and increased local enhancement. Spinal edema in most cases; however, spinal atrophy may be present in the late stages. Although there is no clear evidence in the literature, these patients have been treated in a variety of ways with a course of high-dose steroids, hyperbaric oxygen, anticoagulation, and high-dose vitamin E. Administration of bevacizumab has been shown to improve radiotherapy but with only modest clinical benefit.
Early cancer screening is considered a perfect measure in the timely detection and treatment of all types of cancer. Vinmec International General Hospital currently has a high-tech cancer screening and examination package, including genetic testing, imaging, and biomarkers for early tumor detection. A single gene test can assess the risk of 16 common cancers in both men and women (lung cancer, colorectal cancer, breast cancer, pancreatic cancer, cervical cancer) Bowel cancer , stomach cancer , prostate cancer ,....)
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: Wu J, Ranjan S. Neoplastic Myelopathies. Continuum (Minneap Minn) 2018;24(2, Spinal Cord Disorders):474-496.
MORE:
Vascular diseases of the spinal cord (Part 1) Vascular diseases of the spinal cord (Part 2) Vascular diseases of the spinal cord (Part 3)