This is an automatically translated article.
Posted by Dr. Tran Hoang Ngoc Anh - General Surgery Department - Vinmec Central Park International General Hospital
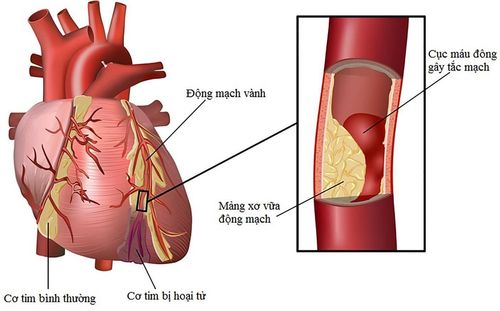
Diseases causing sequelae of muscle spasticity are common: Cerebrovascular accident, traumatic brain injury, spinal cord - spinal cord injury, multiple sclerosis, cerebral motor disability. This patient often presents with spasticity and paralysis of the autonomic muscles because the neurotransmitter structures that coordinate these two manifestations are located in close proximity to each other in the central nervous system.
1. Make a problem
After a central nervous system injury due to various causes can cause sequelae of weakness, spasticity of muscle groups in the limbs, making the patient disabled, creating a real burden for the family and society. Any damage to the central nervous system is followed by a dramatic reorganization of the underlying incompletely lost structures, which is a reorganization of the spinal cord reflexes that control locomotion. body and this explains the spasticity occurrence.
In 1980, Lance first defined spasticity as a movement disorder with a velocity-dependent increase in tone reflexes characterized by hyperactive stretch reflex and this is the type of hypertonia that occurs after damage to the central motor neuron (upper motoneuron). When this spasticity significantly disrupts posture, hindering the rest of the body's movements, the problem of treatment should be raised.
Manifestations spasticity usually occurs after pyramidal lesions due to traumatic brain injury, spinal cord injury and most commonly after cerebrovascular accident with an estimated 18% of spastic sequelae.
In the upper extremities, the common deformity is flexion and contracture of the elbows, wrists and fingers due to spasticity of the biceps, flexor muscles of the arms and hands (Paum dans la main). .
In the lower extremities, one of the most common sequelae of these nerve injuries is spastic equinovarus foot, caused by excessive spasticity of the triceps muscles. triceps surae) located on the back of the lower leg. Excessive spasticity of these triceps limits the flexibility of the ankle joint when walking and consequently alters the patient's gait. Deformity of the horse's foot, whether severe or mild, gradually leads to different functional consequences: sclerosis of the triceps, ankle stiffness, deformity and pain of adjacent joints, gait instability, therefore, to prevent the above consequences, it is necessary to appropriately treat this deformity.
To date, there are many local treatments to reduce spastic deformity of the foot including the use of local injections for neurolysis such as alcohol, phenol, botulinum toxin type A, surgical intervention such as: Neurectomy or selective neurectomy sometimes requires a combination of orthopedic surgery such as tendon extension, tendon transfer...
Among the above methods, elective neurosurgery alone or in combination Orthopedic surgery reduces spastic deformity, helps patients walk and coordinate easily with stable results, lasts longer with low complication rate when compared with injectable methods at the hospital. place. Author Sindou reported that the most common complication was postoperative pain paresthesia, accounting for 12.9%, while this rate was 20% if alcohol block was applied and 30% if phenol was used.
2. Clinical manifestations, diagnosis
Diseases causing sequelae of muscle spasticity are common: Cerebrovascular accident, traumatic brain injury, spinal cord injury, multiple sclerosis, cerebral motor disability. This patient often presents with spasticity and paralysis of the autonomic muscles because the neurotransmitter structures that coordinate these two manifestations are located in close proximity to each other in the central nervous system.
The clinical picture of spasticity can be very diverse due to a variety of factors, the most complete spastic presentation in order include:
Hypertonicity at rest occurs in some cases. Synchronies: Involuntary contractions associated with conscious movements or when examining tendon reflexes, evidence of loss of motor selectivity or an “inhibitory disorder” state. Polydynamic Ia fibers: Alternating action of agonist and antagonist muscles. Increased tendon reflexes: partial manifestation of pyramidal syndrome. Decreased mobility due to paralysis and impaired coordination of muscle control On clinical examination, muscle stiffness is the basic manifestation of spasticity, it is necessary to evaluate the severity, ie the degree of elasticity according to CHARCOT. The spastic limb tends to return to its original position on examination of limb movement. Spasticity occurs predominantly in the postural muscles, in humans spasticity is predominant in the extensors of the lower extremities and in the flexors of the upper extremities (WERNICKE-MANN tone distribution). Other clinical features include:
Loss of tone at rest: At rest, the spastic muscle does not have any contractile activity, all looking like a healthy muscle. Muscle antagonism is proportional to extension velocity: Contraction antagonizes extension, and this resistance increases proportionally to traction velocity. This reflex does not occur at rest and is characterized by increased muscle tone due to causes other than spasticity (in which case the term "stiffness" is often used to describe the muscle). Resistance is lost with prolonged stretching: Spasticity is lost when stretching and keeping the limb in a fixed position for a while (the "tweezers" phenomenon). As the amplitude of extension increases, reflex contracture decreases in the extensor muscles. This phenomenon is explained by the initial role of Golgi receptors in the tendon, followed by the activation of afferent fibers from the secondary neuromuscular spindle, and recently an inhibitory effect on the afferent fibers has been observed. centripetal of the limb flexion reflex. This mechanism does not appear to occur in the upper extremities. Fatigue: Reflexes gradually decrease with repeated stretching. This phenomenon is explained by the gradual depletion of muscle hyperexcitability associated with the depletion of synaptic mediators. Limbs deformity: Upper extremities: Causes contractures in elbows, wrists, fingers. Reducing or losing the function of the hand in daily activities such as stretching the elbow, for the fingers, on the other hand, it is this spasticity that will cause pain, difficulty in personal hygiene, especially in the case of contractures. fingers in the palm (paum dans la main) and finally the aesthetic loss of the hand. Lower extremities: Horse foot deformity is clinically manifest mainly due to triceps sural contracture. This deformity is caused by an imbalance of muscle strength between the overactive triceps on the back of the lower leg and the levator muscles of the foot, mainly the anterior tibialis, with normal or weakened muscle strength. The deformity renders the patient unsteady and forces the patient to walk on tiptoe with the knee overextended or conversely with a compensatory knee flexion. If spasticity of the triceps is accompanied by spasticity of the posterior tibial muscle, in addition to plantar flexion deformities such as horse's foot, there is also a manifestation of internal rotation of the foot (varus). In the same patient, spasticity changes over time, according to different factors such as temperature, physical condition, level of alertness, posture, skin irritation, plant stimulation... on the distribution of injured neuroanatomical pathways.

3. Treatment of muscle spasticity after stroke
Spasticity is only treated when functionally impeded, and with treatment the prognosis is better than no treatment.
Treatment consists of a combination of physical therapy, oral antispasmodic drugs or local injection with Botulinum toxin. When all of the above methods fail, then there will be a role of neurosurgery and orthopedic trauma.
The goal of treatment is to reduce the resulting spasticity such as elbow, wrist, finger, and horse foot contractures. Improve residual limb functions and improve quality of life such as pain relief, self-care, personal hygiene and aesthetics.
Selective microdissection of peripheral nerves:
Principle:
Selective partial resection of motor collateral branches for one or a group of muscles that are evaluated for excessive spasticity. Cutting afferent nerve fibers of spinal cord I (Ia, Ib) reduces muscle spasticity, on motor neuron axons will weaken muscle. However, due to the different recovery of afferent and afferent nerve fibers, long-term control of spasticity is achieved. Selection criteria
Focal muscle spasticity affecting function, failure of oral drug therapy and physical therapy. No active disease requiring medical or other specialized surgical treatment was present. Effective after a local nerve block test. Surgical results:
In practice, it is possible to combine selective nerve ablation in many locations on the same patient, and at the same time coordinate coordinated orthopedic surgery. The state of muscle hypertonia is often improved well after surgery, 70% of patients are satisfied with the results after surgery, improving the rest of the patient's functions, helping with physical therapy, Personal hygiene easier. Surgical complications are usually very low, can cause sensory disturbances in the form of paresthesia, temporary decreased muscle strength after surgery or other common complications such as surgical site hematoma or infection. Vinmec International General Hospital with a system of modern facilities, medical equipment and a team of experts and doctors with many years of experience in medical examination and treatment, patients can rest assured to visit. and stroke treatment at the Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.