This is an automatically translated article.
The article was written by Dr. Tran Truong Giang, Department of Intensive Care, Vinmec Times City International General Hospital.Coronary circulation, cerebral circulation, pulmonary circulation are special types of circulation of the body, which play a very important role in human life.
1. Coronary circulation
Coronary circulation plays an important role in the body, helping to nourish the heart.1.1. Functional anatomical features The coronary artery originates from the aorta, located above the semilunar valve. The coronary artery to the heart is divided into left and right coronary arteries. The left coronary artery is responsible for supplying blood to the anterior left atrium and left ventricle. The right coronary artery supplies blood to most of the right atrium, right ventricle, and posterior left ventricle.
Large arteries are located on the surface of the heart, small arteries go deep into the heart muscle mass and then branch out to form capillaries that run around the myocardium. Branches of a single coronary artery or between branches of multiple coronary arteries are linked together by anastomoses.
Blood when passing through the coronary circulation will provide oxygen and nutrients, then take carbon dioxide and waste products into the coronary veins. Most of the venous blood drains from the left ventricle into the coronary sinus. Blood from the right ventricle passes through the cardiac vein first and then flows directly into the right atrium.
A small amount of blood is poured directly into the heart chambers through the Thebesian veins. Alternatively, blood can also flow directly from the coronary arterioles into the heart chambers (Figure 13).
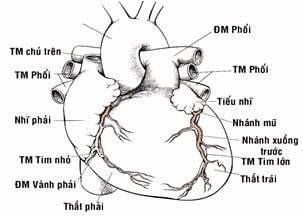
Hình 13: Động mạch vành và các nhánh
At the beginning of systole, when blood pressure increases suddenly, the blood speed also increases. When the ventricles contract, the blood pressure remains high, but the rate decreases. When the heart muscle contracts, it will press on the blood vessels in the heart muscle mass, causing the arteries to narrow, so the pressure increases but the speed is slow.
At the diastolic stage, the heart muscle relaxes, the coronary vessels will dilate, the pressure decreases but the speed increases, the blood in the coronary arteries flows more easily. Thus, during diastole, coronary circulation is rapid and abundant. Systolic and coronary circulation will be slow and less.
Coronary flow at rest is about 255ml/min, accounting for 4-5% of cardiac output. When exercising, the cardiac output will increase 4 to 6 times, the work of the heart will increase 6 to 8 times, the coronary flow will also increase 4 to 5 times to supply nutrients to the heart.
Thus, coronary flow increases but is not commensurate with the increase in cardiac work. Therefore, the heart must increase energy efficiency to minimize the lack of blood supply in muscle.
In addition, coronary flow also changes with the heart's cycle. Coronary outflow is reduced during systole, as the left ventricular muscle presses against the intramuscular blood vessels during contraction. In contrast, during diastole, the heart muscle relaxes completely, allowing blood to flow more easily and faster.
1.3. Coronary circulatory regulation 1.3.1. Humoral factors The local nutritional requirement of the myocardium helps to regulate blood flow through the coronary circulation. To regulate coronary circulation, oxygen demand is the main factor. When oxygen levels in the heart decrease, heart muscle cells release vasodilators, which dilate the arterioles, allowing more blood to flow. Adenosine is the most important substance and some other substances such as K+, H+, carbonic, bradykinin, prostaglandin.
1.3.2. Nerve factors Autonomic neuropathy stimulates the heart, affecting coronary flow in two ways: directly and indirectly. The direct effect occurs by the action of neurotransmitters such as norepinephrine and acetylcholine on the coronary arteries.
Indirect effects occur due to secondary changes in coronary flow depending on the degree of increase or decrease in cardiac output. Sympathetic stimulation increases heart rate, contractility, and metabolic rate. An increase in cardiac activity causes oxygen levels in the heart muscle to decrease and dilates coronary arteries.
In contrast, parasympathetic stimulation causes the heart rate to slow down, the heart's activity to decrease. As a result, the myocardium will reduce oxygen consumption causing coronary vasoconstriction.
Sympathetic neurotransmitters can cause vessels to constrict or dilate, depending on the presence or absence of specific receptors on the blood vessel wall. A receptor causes vasoconstriction while B receptor causes vasodilation.
These two types of receptors are found in coronary vessels, A receptor mainly appears in blood vessels adjacent to the pericardium. The B receptor is mainly present in the arteries in the myocardium. Therefore, sympathetic stimulation can cause coronary contraction or dilation.
Metabolic factors, especially oxygen consumption, play a major role in the regulation of coronary flow. Therefore, when nerve stimulation alters coronary flow, metabolic factors return flow to normal levels.
2. Brain Circulation

Nếu não chỉ thiếu oxy trong vài giây thì người bệnh sẽ mất ý thức
Therefore, blood flow to the brain is normally maintained at approximately 750 mL/min, representing 15% of the resting cardiac output.
2.1. Functional anatomical features There are four arteries that supply the brain with blood: two vertebral arteries and two internal carotid arteries. The vertebral arteries join together to form the basilar artery. The ring of Willis is formed from the basilar artery and two internal carotid arteries.
This is the starting point of 6 large blood vessels, which play an important role, supplying blood to the brain. The arteries that feed the brain, when reaching the cerebral cortex, have interconnecting vessels, and when necessary, these branches will form the supporting circulation.
Veins have almost no muscle fibers and have very thin walls. While the cerebral veins run on the cortical surface, the cerebral arteries are located deep. The veins are connected, without valves, so blood can return to the heart in two directions in the veins. Cerebral venous blood flows to the two internal jugular veins, and then back to the heart.
Cerebral circulation takes place entirely in the skull, does not expand. Therefore, changes in blood volume in the brain can only occur with opposite changes in volume in another part, usually the cerebrospinal fluid.
2.2. Blood dynamics in cerebral circulation The pressure of the cerebral arteries is about 83-85 mmHg and varies with position. During each stroke, blood pressure and brain will be greatly reduced thanks to the anatomical structure. Cerebral arterial blood pressure will change according to fluctuations in systemic blood pressure. This range can range from 60 mmHg to 140 mmHg without altering cerebral flow.
Normally, blood flow through the brain is stable around 750ml/min and barely changes as the heart changes.
2.3. Regulation of cerebral blood flow 2.3.1. Autoregulation When the pressure in the systemic arteries increases, more blood flows to the brain, causing the cerebral blood vessels to constrict, and less blood to the brain. Conversely, when the pressure in the systemic arteries decreases, less blood flows to the brain, and the cerebral vessels dilate to allow more blood to reach the brain. This self-regulation helps maintain a constant blood flow at rest, during exercise, or during emotions.
2.3.2. Humoral factors Cerebral blood vessels are quite sensitive to the carbon dioxide concentration in the arteries. When the amount of carbon dioxide increases, due to decreased ventilation, the cerebral arterioles will dilate, causing increased cerebral blood flow.

Mạch máu não khá nhạy cảm với nồng độ khí carbonic trong động mạch
The decrease in oxygen pressure in the cerebral arteries causes increased cerebral blood flow, vasodilation and increased oxygen supply. When oxygen pressure drops, brain function is immediately disrupted.
2.3.3. Nervous factor Sympathetic stimulation of the large vessels is slightly constricted but does not affect the small blood vessels. Parasympathetic stimulation also causes mild vasodilation. Thus, the autonomic nervous system has almost no important role in the regulation of cerebral blood flow.
Only when mean arterial pressure rises to 200 mmHg can the sympathetic nervous system induce cerebral vasoconstriction, which protects arterioles from stress rupture and stroke.
3. Pulmonary circulation
Pulmonary circulation, also known as microcirculation, has the function of bringing venous blood from the heart to the lungs, exchanging gases with the alveoli, exhaling carbon dioxide, receiving oxygen, and returning blood to the left heart.The microcirculation is a functional circulation, not a nutrient circulation. The function of feeding the lungs is provided by the bronchial artery, a branch of the aorta.
3.1. Structural and functional features The right ventricle has the function of carrying blood through the pulmonary artery, along the left and right branches, helping to bring blood to the two lungs. From there, it helps to branch out into smaller branches, reaching the terminal bronchioles, forming the pulmonary capillary network. Pulmonary capillaries are the site of gas exchange. The blood then follows the pulmonary veins to the left atrium.
Pulmonary artery wall is quite thin, contains less upper muscle fibers, so it has the ability to dilate more than the aorta. The pulmonary circulation capillaries are short but have a very wide cross-section, with many connections, facilitating gas exchange. Pulmonary circulation takes place in the thoracic cavity, under negative pressure, pulmonary blood vessels will dilate relatively, helping blood circulate quickly.
3.2. Blood dynamics in the pulmonary circulation Blood flowing in the pulmonary circulation also flows from areas of high pressure to areas of low pressure. Pulmonary artery pressure is lower than systemic circulation, with systolic/diastolic values of 25/10mmHg and mean pressures of 15mmHg.
Such low pressure is because blood from the right ventricle encounters very little resistance, so it is possible to push the same amount of blood as the left ventricle with less work.
To determine the pressure in the right heart chamber to the pulmonary capillaries, doctors will use the right heart catheterization technique. Pulmonary capillary pressure is about 10 mmHg, when this pressure increases above 25 mmHg, it will cause congestion and pulmonary edema. Pulmonary venous pressure and left atrial pressure are equal, about 0-2 mmHg.
Although the blood pressure is lower, the pulmonary resistance is weak, so the blood flow through the two circulations is equal. The amount of blood contained in the pulmonary circulation is only about 450ml (accounting for 9% of the whole body's blood volume), so the blood velocity in the primary circulation must be higher than that in the macrocirculation.
The blood velocity in the aorta and pulmonary artery is equal, so the blood velocity in the pulmonary capillaries must be faster than the blood velocity in the macrocirculatory capillaries, due to the wider diameter of the pulmonary capillaries and the blood in the capillaries The lungs do not experience strong resistance.
3.3. Pulmonary Blood Flow Regulation Pulmonary blood flow is equal to cardiac output, so cardiac outflow regulators, mainly peripheral factors, also regulate pulmonary outflow. In the pulmonary circulation, it is important that blood is distributed to the areas of the lungs where the alveoli are best oxygenated.
Lượng máu qua phổi bằng lưu lượng tim nên yếu tố điều hòa lưu lượng tim
Meanwhile, in the systemic circulation, capillaries dilate in the absence of tissue oxygen, but are very useful for pulmonary circulation. In poorly ventilated areas, where gas exchange is low, blood will not come.
When the oxygen pressure in the alveoli increases, the surrounding blood vessels dilate, blood to the lungs also increases. When breathing in, the alveoli are filled with gas, the high oxygen pressure helps the pulmonary vessels to dilate, allowing blood to flow to the lungs easily. When the alveoli are full of gas, the capillaries are also filled with blood, which is favorable for gas exchange in the alveoli. Self-regulating pulmonary circulation will help distribute blood to different regions of the lungs in proportion to their ventilation levels.
Besides, when the X wire is stimulated to the lungs, the pulmonary vascular resistance will be slightly reduced, the blood volume to the lungs will increase. Sympathetic stimulation causes a relative increase in pulmonary vascular resistance.
Vinmec International General Hospital is one of the hospitals that not only ensures professional quality with a team of leading medical doctors, modern equipment and technology, but also stands out for its examination and consultation services. comprehensive and professional medical consultation and treatment; civilized, polite, safe and sterile medical examination and treatment space.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.