This is an automatically translated article.
Posted by Dr. Truong Ngoc Hai - Resuscitation Doctor - Emergency Department - Vinmec Central Park International General HospitalDuring artificial ventilation (ventilator), the patient is assisted in ventilation by the introduction of an air-oxygen mixture into the patient's lungs. Through an endotracheal tube or tracheostomy tube (invasive ventilation) or through a mask (non-invasive ventilation) until the patient is able to breathe effectively on his own.
1.Artificial ventilation During artificial ventilation, a predetermined mixture of air (i.e. oxygen and other gases) is pushed into the central airways and then flows into the alveoli. As the lungs stretch, the pressure in the alveoli increases. When the ventilatory goal is reached (usually volume or pressure, sometimes airflow) the ventilator stops delivering air to the central airway and central airway pressure decreases. Passive expiration due to the pressure difference between the thorax and the ventilator's artificial airway
2. When should a patient be on Artificial Ventilation (ventilator)? During surgery: Ventilators can temporarily assist in ventilation of the patient while the patient is under general anesthesia.
Recovery from surgery: Sometimes patients need a ventilator to help them breathe for a few hours or even days after surgery.
When breathing is difficult: The patient should be helped to breathe on a ventilator if the patient has a serious lung disease or a medical condition that makes it difficult or impossible to breathe effectively on his own:
The condition affects the patient's breathing. alveolar filling process: pneumonia – bacterial infection, aspiration; noncardiac pulmonary edema/ARDS (due to NK, lung injury from aspiration, drowning, blood transfusion, pulmonary contusion); Cardiac pulmonary edema, pulmonary bleeding, alveolar pathology
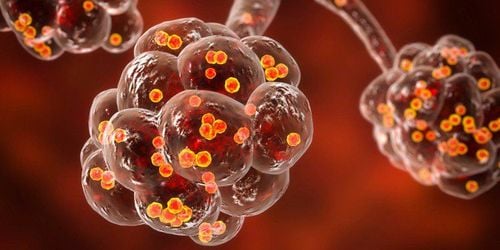
Bệnh viêm phổi do nhiễm khuẩn có thể làm đầy các phế nang
Pulmonary vascular disease: pulmonary infarction, amniotic fluid embolism, cancer embolism Pathology causing central airway obstruction: tumor, oropharyngeal, laryngeal edema, tracheal stenosis Pathology causing distal airway obstruction : COPD, obstructive airway disease, bronchial asthma Hypoventilation due to compromised respiratory control: general anesthesia, drug overdose, poisoning Hypoventilation due to dysfunction of respiratory muscles, systemic peripheral nerves: amyotrophic lateral sclerosis, myasthenia gravis, guillain barre, strychnine poisoning, muscle atrophy, hypotonic muscle atrophy, myositis Hypoventilation due to pathology of the chest wall, pleura: thoracic malformation, Massive pleural effusion, pneumothorax Pathology with increased need for ventilation: severe infection, septic shock, severe metabolic acidosis. 3. When does the patient have a contraindication to artificial ventilation (ventilator)? Absolute contraindication : Undrained pneumothorax
Relative contraindication:
Patient and/or family disagree Medical condition unsuitable for emergency effort. Example: end-stage malignancy, DNR (do not resuscitate) patient 4. Common invasive modes of ventilation in ICU Assisted Control (AC): ventilator providing a minimal respiratory rate With minimal presets, the patient self-activates additional breaths with full machine support. Tachypnea can cause respiratory alkalosis and auto-PEEP.
Synchronous intermittent controlled artificial ventilation (SIMV): ventilator that provides a minimum respiratory rate that is in sync with the patient's breathing effort. The patient's additional breaths may not be supported (depending on whether or not combination mode is used), but the patient needs to overcome wiring resistance during spontaneous breathing. SIMV = AC when patient has no spontaneous breathing effort
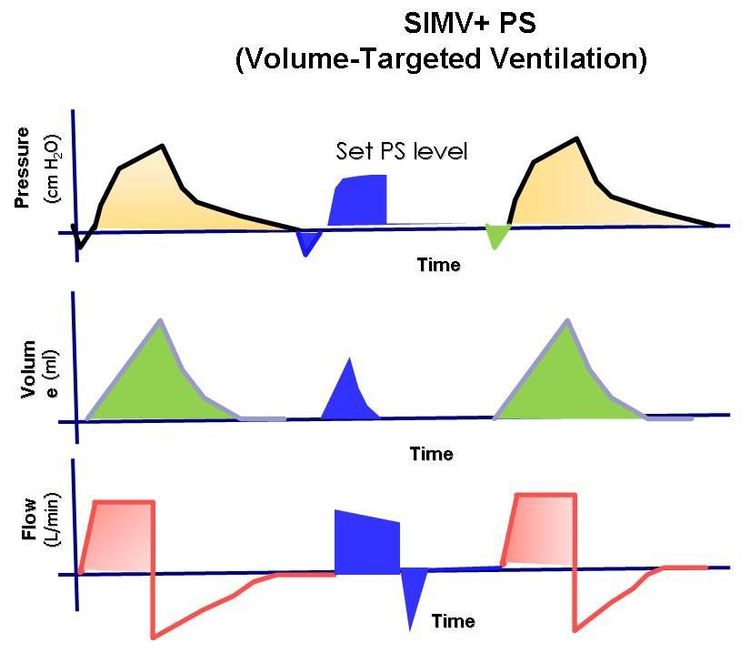
Áp suất, âm lượng và lưu lượng theo dạng sóng thời gian để thông gió bắt buộc gián đoạn đồng bộ (SIMV).
Continuous positive airway pressure: the patient breathes spontaneously when the ventilator maintains a constant positive airway pressure.
5. Implementation process
Step 1: Carry out endotracheal intubation if the patient has not been intubated or has not had a tracheostomy. Squeeze the oxygen balloon through the endotracheal tube while preparing the ventilator. Step 2: Set initial ventilator parameters Step 3: Set alarm limits Step 4: Set alarm limits, set levels depending on the specific medical condition of each patient. Step 5: Carry out ventilation for the patient. Adjust ventilator parameters 6. What are the risks of artificial ventilation? Artificial ventilation can contribute to saving the patient's life. However, like other treatments, there can sometimes be some risks and complications with artificial ventilation. The risk increases if the patient is on the ventilator for a long time.
6.1 Risk of infection A common risk of artificial ventilation is infection. Patients may have ventilator-associated pneumonia. Infection of the sinuses can also occur. The patient needs antibiotics to treat pneumonia or an infection in the sinuses.
6.2 Irritation, irritation The endotracheal tube or tracheostomy tube can rub and irritate the patient's airway. An endotracheal tube or tracheostomy tube can also make coughing difficult. The cough response helps to remove phlegm and irritants from the patient's lungs.

Ống nội khí quản hoặc canuyn mở khí quản có thể gây khó chịu cho người bệnh
6.3 Injury to vocal cords, larynx The endotracheal tube passes through the pharynx, vocal cords, and larynx. This is why the patient cannot talk while on the ventilator. During mechanical ventilation, vocal cord and larynx injuries may occur related to long-term endotracheal intubation and/or patient stimulation and struggle.
6.4 Lung injury During mechanical ventilation, lung damage can occur, for a number of reasons:
Alveoli inflate due to increased pressure in the lungs Pneumothorax (air leaks into the pleural space). between the lungs and chest wall) Oxygen toxicity (must use high concentrations of oxygen) 6.5 Other possible hazards include: Skin, soft tissue infections Embolism, pulmonary embolism due to blood clots
Artificial ventilation is performed at Vinmec International General Hospital with a highly configured ventilator system for ICUs for adults, children and infants.
In particular, the team of doctors performing the technique are all doctors in the Emergency Department with high professional experience:
To register for examination and treatment at Vinmec International General Hospital, you You can contact Vinmec Health System nationwide, or register online HERE.