This is an automatically translated article.
The article was consulted with Specialist Doctor I Le Thi Thu Hang - Dermatologist - Department of Medical Examination & Internal Medicine - Vinmec Hai Phong International General Hospital.The skin is one of the largest organs in the body in terms of surface area and weight. The skin consists of two main layers: the epidermis and the dermis. The skin has three main functions: protection, temperature regulation, and sensation. Wounds affect all functions of the skin. This article helps you better understand the structure of the skin, its layers and roles.
1. Structure and role of the skin
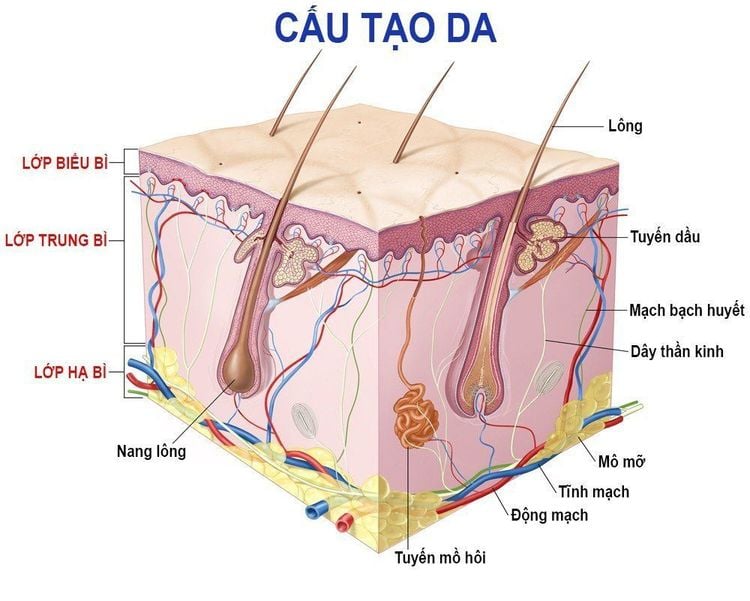
1.1. Skin structure The skin is composed of many different layers:Epidermis: is the outermost layer of skin, the epidermis consists of 5 cell layers: basal layer, spiny layer, granular layer, gloss layer and stratum corneum. Dermis: Consists of papillary and reticular layer Subcutaneous layer: consists of fatty tissue. It also contains Vater-Pacini corpuscles (receptors) and hair follicles. 1.2. The role of the skin * The main functions of the skin include:
- Protecting the body against all external agents such as:
+ Muscle, heat, other physical trauma
+ Harmful agents
+ Loss too much moisture and vitamins
+ Harmful effects of radiation and UV rays
- Regulating body temperature: One of the important functions of the skin is to protect the body from cold or heat and maintain body temperature unchanged. This is achieved by altering the blood flow through the vascular layer of the skin. During warm periods, the vessels dilate, the skin reddens, and sweat particles form on the surface (vasodilation = more blood flow = more direct heat loss). During cold periods, blood vessels constrict, preventing heat from escaping (vasoconstriction = less blood flow = reduced heat loss). The excretion and evaporation of sweat from the surface of the skin also helps to cool the body.
- Sensing painful and pleasant stimuli: The skin is a 'tactile' organ that triggers a response if we touch or feel something, including things that can cause pain. This is important for patients with skin conditions, as many can experience pain and itching and a reduced quality of life.
In addition, the skin also has an aesthetic function, creating a very important appearance in daily life and communication.
- Immunological surveillance: The skin is an important immune organ, made up of important structures and cells. Depending on the immune response, many types of cells and chemical messengers (cytokines) are involved.
- Biochemical function: The skin is involved in a number of biochemical processes. In the presence of sunlight, a form of vitamin D called cholecalciferol is synthesized from a derivative of the steroid cholesterol in the skin. The liver converts cholecalciferol to calcidiol, which is then converted to calcitriol (the active chemical form of the vitamin) in the kidneys. Vitamin D is needed for the normal absorption of calcium and phosphorus, which is necessary for healthy bones. The skin also contains receptors for other steroid hormones (oestrogens, progestogens and glucocorticoids) and vitamin A.
- Social and sexual functioning: People make judgments based on what they see and can form their first impression of someone based on how that person looks. Throughout history, people have been evaluated for their skin, such as by color or the presence of skin conditions or scars. Doctors will evaluate many signs of disease based on your skin.
The skin stores important chemicals and nutrients in the body while providing a barrier against dangerous substances entering the body and protection from the harmful effects of ultraviolet radiation emitted by the sun. Additionally, skin tone, texture, and folds help mark people as individual. Anything that interferes with skin function or causes changes in appearance can have major consequences for physical and mental health.
Many skin problems are limited to the skin. Sometimes, however, the skin provides clues to a disorder that affects the entire body. As a result, doctors often have to consider many possible conditions when evaluating skin problems. They may need to order blood tests or other lab tests to look for medical problems in people who have skin problems with them.
2. Layers of skin
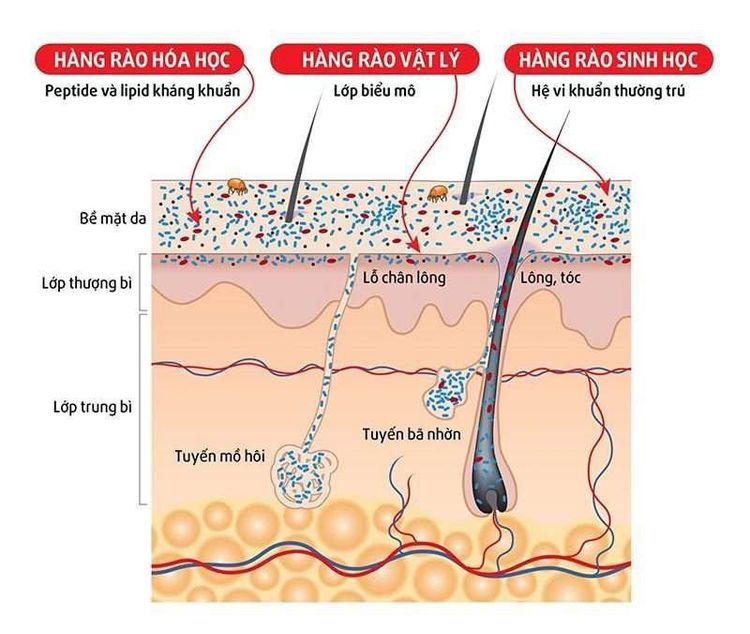
2.1. Epidermis The epidermis is the outermost layer of the skin, defined as the stratified squamous epithelium, mainly composed of keratinocytes in the stages of advanced differentiation. Keratocytes produce the protein keratin and are the major building blocks (cells) of the epidermis. Since the epidermis is avascular (contains no blood vessels), it is completely dependent on the underlying dermis to distribute nutrients and waste waste across the basement membrane.The main function of the epidermis is to act as a physical and biological barrier to the external environment, preventing the entry of irritants and allergens. At the same time, it prevents water loss and maintains homeostasis. The epidermis is composed of layers; Most body parts have four layers, but people with the thickest skin have five layers.
Skin cells include:
- Keratinocytes produce keratin (tough fibrous protein). Keratocytes are formed by division in the basal layer. As they move up through the spiny and granular layers, they differentiate to form a rigid internal structure of keratin, microfilaments, and microtubules (keratinisation). The outer layer of the epidermis, the stratum corneum, consists of flattened layers of dead cells that have lost their nucleus. These cells are then shed from the skin (scabs); This complete process takes about 28 days.
Between these keratinocytes there is a complex mixture of lipids and proteins. These intercellular lipids are degraded by keratinocyte enzymes to produce a lipid mixture of ceramides (phospholipids), fatty acids, and cholesterol. These molecules are arranged in a highly organized fashion, combining with each other and the keratinocytes to form the lipid barrier of the skin against water loss and the entry of allergens and irritants.
The stratum corneum can be visualized as a brick wall, with the keratinocytes forming the brick and the lipid layers forming the mortar. Since the keratinocytes contain water retention - a natural moisturizing factor - they attract and retain water. The high water content in the keratinocytes causes them to swell, keeping the stratum corneum supple and elastic, and preventing the formation of cracks and fissures. This is an important note when applying topical medications. They are absorbed across the epidermal barrier into the underlying tissues and structures (absorbed through the skin) and transported to the circulatory system.
The stratum corneum regulates the amount and rate of absorption through the skin. One of the most important factors affecting this is skin moisture and environmental humidity. In healthy skin with normal hydration, the drug can only penetrate the stratum corneum by passing through the tight, relatively dry lipid barrier between cells. When moisture is increased in the skin or the normal barrier of the skin is impaired due to skin disease, peeling, abrasion, chafing or premature birth, absorption through the skin is increased.
- Melanocytes : these cells produce dark skin pigment. Melanocytes are found in the basal layer and are scattered among the keratinocytes along the basement membrane with a ratio of one melanocytes to 10 basal cells. They produce the pigment melanin, which is produced from tyrosine, which is an amino acid, which is packaged in cell vesicles called melanosomes, and transported and distributed into the cytoplasm of keratinocytes. The main function of melanin is to absorb ultraviolet (UV) radiation to protect us from its harmful effects.
Skin color is not determined by the number of melanocytes but by the number and size of melanosomes. It is affected by a number of pigments, including melanin, carotene, and hemoglobin. Melanin is transferred into keratinocytes via melanosomes. Therefore, the color of the skin depends on the amount of melanin produced by the basal melanocytes and received by the keratinocytes.
Melanin occurs in two main forms:
+ Eumelanin: exists as black and brown
+ Pheomelanin: produces red
Skin color is also affected by exposure to UV radiation, genetic factors and photos hormonal effects.
- Merkel cells: are associated with sensory nerve endings. These cells are present only in very small numbers in the basal layer. They are closely associated with cutaneous nerve endings and appear to play a role in sensation, particularly in areas of the body such as the palms, soles, and genitals.
- Langerhans cells: macrophage-like dendritic cells. These are cells that represent antigens (microorganisms and foreign proteins) found in the spiny layer. They are part of the body's immune system and constantly monitor for antigens in their surroundings so they can trap them and present them to T-helper lymphocytes, thereby triggering an immune response.
The keratinization of the epidermis is a continuous process. The cells needed for this constant renewal come from the basal layer where cell division takes place. Since this process is very sensitive to radiation, there are pigments in the germ layer that create a protective layer of skin that darkens when exposed to strong sunlight.
On the other hand, the stratum corneum is very thin where greater flexibility is required, such as on the eyelids. In places exposed to mechanical stress, like the palms of the hands or soles of the feet, it thickens and can form calluses. The formation of calluses is a defense mechanism. As soon as the impacts subside, the formation of thicker layers stops.
Nerve endings sense pain, touch, pressure, and temperature. Some areas of the skin contain more nerve endings than others. For example, the tips of the fingers and toes contain many nerves and are extremely sensitive to touch.
Sweat glands secrete sweat in response to heat and stress. Sweat is composed of water, salt, and other chemicals. As sweat evaporates from the skin, it helps cool the body. Specialized sweat glands in the armpits and genital areas (apocrine sweat glands) secrete oily, thick sweat that produces a characteristic body odor when the sweat is digested by skin bacteria in those areas.
The sebaceous glands secrete sebum into the hair follicles. Sebum is an oil that keeps the skin moist and soft and acts as a barrier against foreign substances.
Hair follicles give rise to many different types of hair throughout the body. Hair not only contributes to a person's appearance, but also has a number of important physical roles, including regulating body temperature, protecting from damage, and enhancing sensation. Part of the cyst also contains stem cells that have the ability to regrow damaged epidermis.
The blood vessels of the dermis provide nutrients to the skin and help regulate body temperature. Heat causes blood vessels to dilate (dilate), allowing large amounts of blood to circulate near the surface of the skin, where heat can be released. Cold causes blood vessels to narrow (constrict), keeping the body warm.
In different parts of the body, the number of nerve endings, sweat and sebaceous glands, hair follicles and blood vessels varies. For example, the top of the head has many hair follicles, while the soles of the feet have none.
Fat layer
Below the dermis is a layer of fat that helps insulate the body from heat and cold, provides a protective cushion and acts as an energy storage area. Fat is contained in living cells, called adipocytes, which are held together by fibrous tissue. The layer of fat varies in thickness, from a fraction of an inch above the eyelids to several inches above the belly and buttocks in some people.
3. Glands of the skin
Sebaceous glands: Sebaceous glands are located in the dermis. They can be found almost anywhere on the human body, except for the palms of the hands and soles of the feet. Normally, the sebaceous gland is located right next to the hair follicle. This means that a sebaceous gland merges into the excretory duct of the hair follicle. This junction does not exist on the eyes and eyelids, nor does it exist on the lips, penis, or labia. Sebum itself consists of:+ Cholesterol
+ Protein
+ Electrolytes
Earwax (cerumen) is also a product of the sebaceous glands. Sebum repels water and lubricates hair and skin.
- Sweat glands: The human body has about 2-3 million sweat glands (eccrine glands), located in the dermis. Their excretory ducts follow a tortuous path, ending in skin pores. They are found mainly in the armpits, soles, and palms. Sweat not only contributes to temperature regulation, but also plays a protective role in the skin. Its pH value is 5–6. Sweat production is affected by many factors; among others are psychological ones like stress.
- Scent glands: Scent glands (also known as apocrine sweat glands) are located mostly in the armpits, around the nipples, and in the genitals. They play an important role in creating a person's unique body odor, which is influenced by other factors, such as sweat or bacteria on the skin.
4. Skin appendages
Hair and nails are also considered part of the skin, i.e. the connective system. As such, they are called skin appendages.4.1. Hair - protective and tactile organ Hair has many different functions. It serves as protection against the cold and as an important organ of touch.
Hair growth begins in the dermis, more specifically in the hair papilla. Hair consists of keratinized cells that emerge and migrate up inside the hair follicle. As the hair emerges from the surface of the skin, it will do so at a slight angle. For each hair follicle, there is an adjacent sebaceous gland and usually an odor gland.
Hair can stand up thanks to the action of muscles, that's what happens when you get a 'chill down your spine'. It is a very old function of the human body that cannot be changed in a state of 'goosebumps' (cutis anserina). Moreover, the nerve fibers present in the hair make the hair very susceptible to touching each other.
Hair growth: In infants, the entire body is covered with a very fine layer of hair called vellus hair. During puberty, head hair begins to grow, much thicker and mainly in certain areas of the body, such as the genital area or face (beard). The rest of the body hair is less pronounced and 4% of the skin surface is not covered by hair including:
+ Palms
+ Palms
+ Fingernails
+ Toenails
+ Lips
These This hairless part of the skin is called the glacial skin, in contrast to the hairy skin.
Hair grows about 1cm per month. The growth cycle is divided into 3 phases.
- Phase 1 lasts 2–10 years. It is called the growth phase or anagen phase.
- Phase 2 lasts about 2 weeks. It is called the transition phase or the catagen phase.
- Stage 3 lasts about 3–8 months. It is called the resting phase or the telogen phase.
These stages are defined for a hair follicle that goes through this cycle up to 10 times. After that, it doesn't form any more hairs. A healthy person loses up to 100 hairs per day.
4.2. Nails - protective and grasping organs Nails are made of hard, dense keratinized cells of the epidermis. They fulfill an important task of being able to grasp small objects, similar to the operation of tweezers. Furthermore, they act as an important protective layer of the fingertips and toes against injury. Translucent nails. The light pink color that shines through is that the nail is well supplied with blood.
The end of the white crescent-shaped nail (towards the body) is called the lunula ('little moon'). Here the actual white color of the nail can be appreciated as the nail is not transparent in this part. Between the spines and the skin, there is a protective layer called the epidermis, which prevents germs from entering. Behind the cuticle (towards the stem) there is the nail base. It forms keratinized cells that push the nail forward. Fingernails grow faster than toenails. Typical nail growth rate is 1 mm per week; Toenails grow by 0.5 mm per week.
The structure of the nail:
- Nail plate: surface of the sebaceous glands
- Nail layer: continuous with layers of basale and spinosum
- Nail base: covering the germination area or substrate
- Eponychium (layer) cuticle)
- Hyponychium
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: merckmanuals.com, byjus.com, nursingtimes.net













