This is an automatically translated article.
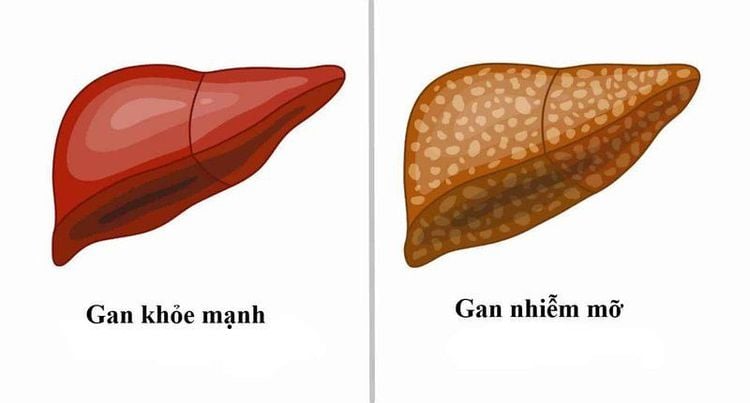
Nonalcoholic fatty liver disease (NAFLD) is a general term for liver conditions that affect people who drink little or no alcohol. The main feature of nonalcoholic fatty liver is that too much fat is stored in the liver cells. Read more articles below to understand more about signs of nonalcoholic fatty liver.
1. What is non-alcoholic fatty liver?
Non-alcoholic fatty liver disease (NAFLD) is extra fat that builds up in liver cells that aren't caused by alcohol. The normal liver contains some fat. However, if more than 5-10% of the weight of the liver is fat, it is called fatty liver.
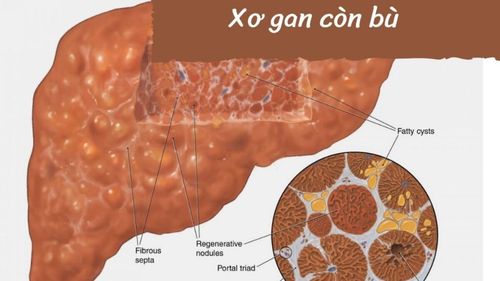
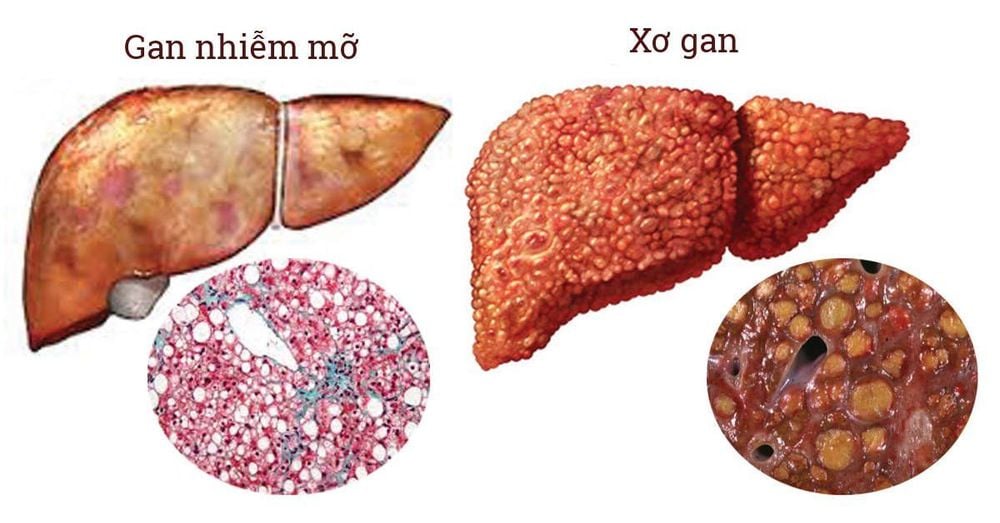
Non-alcoholic fatty liver disease is divided into 2 main groups, namely: non-alcoholic fatty liver (NAFL) or (2) non-alcoholic fatty liver disease (non-alcoholic fatty liver disease). steatohepatitis (NASH), is characterized by hepatocellular degeneration, lobular inflammation with or without periportal fibrosis, which can eventually lead to cirrhosis and cancer.
Non-alcoholic fatty liver disease alone has a higher risk of leading to fibrosis, cirrhosis than NAFLD and liver cancer. Usually patients develop one type of nonalcoholic fatty liver disease or another, but sometimes people with one form are later diagnosed with another form of NAFLD.
Nonalcoholic fatty liver disease is simply a form of nonalcoholic fatty liver disease in which you have fat in your liver but in small amounts, without causing inflammation or damage to the liver. Nonalcoholic fatty liver disease alone usually does not progress, so it will not cause complications or damage to the liver. However, nonalcoholic fatty liver disease alone causes the liver to enlarge, which causes pain.
gan nhiễm mỡ
Nonalcoholic steatohepatitis is a form of NAFLD in which your liver is already inflamed and damaged, and there is certainly fat in the liver. The inflammation and liver damage of NASH can cause fibrosis or scarring of the liver. Nonalcoholic steatohepatitis can lead to cirrhosis, scarring, and permanent damage. Cirrhosis can lead to externally linked NIH liver cancer. NASH is diagnosed most often in patients aged 40 to 60 years but can occur in any age group.
2. Causes of Nonalcoholic Fatty Liver Disease Fatty liver develops for a variety of reasons, involves multiple biochemical mechanisms, and causes different forms of liver damage. Pathophysiology involves fat accumulation (steatosis), inflammation and possibly, fibrosis. Fatty is the result of a buildup of triglycerides in the liver. Possible mechanisms of steatosis include decreased synthesis of very low-density lipoprotein (VLDL) and increased hepatic triglyceride synthesis (possibly due to decreased fatty acid oxidation or increased free fatty acids released by the liver). delivered to the liver). Inflammation may result from lipid peroxidation damage to cell membranes. These changes can stimulate existing astrocytes in the liver, leading to fibrosis. If advanced, NASH can cause cirrhosis and portal hypertension.
Causes of nonalcoholic fatty liver include:
Overweight, obesity: Obesity is one of the most important causes of nonalcoholic fatty liver disease. 70% of obese people suffer from this condition due to obesity. Fatty liver disease is known to affect the body's ability to process fat and lose weight. As a result, you continue to gain weight and develop nonalcoholic fatty liver disease. This often happens to people who have a high-fat diet and don't exercise. Insulin resistance: There seems to be an important link between NAFD and insulin resistance. Insulin helps your muscles and tissues get glucose from your blood for energy. It also helps the liver store excess glucose. When a person has insulin resistance, their body does not respond to insulin the way it should. As a result, excess fat is stored in the liver leading to inflammation and scarring. Metabolic syndrome: Having metabolic syndrome or any of its features is also thought to be the cause of non-alcoholic fatty liver disease. It refers to a group of conditions or characteristics associated with obesity. People with this condition are more likely to develop heart disease and type 2 diabetes. Doctors say a person with metabolic syndrome can have any of these three signs: Large waist size high blood triglycerides, high blood sugar level, high blood pressure, low HDL cholesterol, have diabetes. Excess fat in the blood: High levels of fat, triglycerides and bad cholesterol in the blood are also an important cause of nonalcoholic fatty liver disease. When the body becomes resistant to insulin, the liver begins to take fatty acids from the blood, which is rich in fatty acids. As a result, this fat begins to accumulate in the liver as stored fat. It also kills the liver's ability to remove excess fat from the body. This then develops into fatty liver disease. Theoretically, fatty liver is divided into 4 degrees:
Grade 0: The amount of fat in the liver is less than 5% of the weight of the liver; Grade 1: the amount of fat in the liver is from 5% to less than 33% of the weight of the liver; Grade 2: Fat in the liver from 33% to less than 66% of the weight of the liver; Grade 3: Fat equal to or greater than 66% of the weight of the liver. In clinical practice, the degree of hepatic steatosis is usually determined by ultrasound or liver elastography. In case of necessity, computerized tomography, magnetic resonance imaging, liver biopsy can be added.
Gan nhiễm mỡ do nhiều nguyên nhân gây ra.
3. Signs of non-alcoholic fatty liver Fatty liver is a disease that progresses silently, often without any symptoms. As a result, the disease is often discovered incidentally during blood tests, ultrasound, or liver elastography. Some cases have symptoms of fatigue, loss of appetite, right lower quadrant pain, slightly enlarged liver, pressure.
Most NAFLD patients do not have any symptoms. However, some patients with NASH complain of fatigue and vague discomfort in the upper right region of the abdomen.
Usually, patients with NAFLD are noticed because elevated levels of liver transaminases are revealed in a blood sample or because fatty infiltration of the liver is discovered incidentally on ultrasound or radiographic examination such as CT scan. computer class (CT). Sometimes hepatomegaly can be detected during a physical exam.
4. Confirm the diagnosis of nonalcoholic fatty liver 4.1. Blood tests The diagnosis of NASH should be suspected in patients with the metabolic syndrome (obesity, type 2 diabetes, hypertension, or dyslipidemia) and in patients with laboratory abnormalities. unexplained liver disease. Distinguishing steatosis alone from NASH can be difficult, and elevated liver enzymes are not a sensitive predictor of NASH. The presence of metabolic syndrome as well as elevated ferritin increases the likelihood that the patient has NASH rather than steatosis alone. Furthermore, clinical scoring systems such as the FIB4 score, the NAFLD fibrosis score calculator or the NASH FibroSure® in the laboratory can identify patients who are at risk for fibrosis and therefore who are more likely to develop fibrosis. have NASH and are at risk of progression to cirrhosis. When liver enzymes are elevated, the most common laboratory abnormalities are elevated aminotransferase levels. Unlike in alcohol-related liver disease, the ratio of aspartate aminotransferase (AST) to alanine aminotransferase (ALT) in NASH is usually < 1. Alkaline phosphatase and gamma-glutamyl transpeptidase (GGT) are sometimes increased. Hyperbilirubinemia, prolonged prothrombin time (PT), and hypoalbuminemia are uncommon.
4.2. Liver biopsy A liver biopsy is the only test that can confirm the diagnosis of NASH and indicate the severity of the disease. Liver biopsies may show fibrosis at an earlier stage than liver biopsies. However, doctors do not recommend a liver biopsy for everyone with suspected NAFLD.
Your doctor may recommend a liver biopsy if you are more likely to have NASH with advanced fibrosis or if your other tests show signs of advanced liver disease or cirrhosis. In some cases, your doctor may recommend a liver biopsy to rule out other liver diseases. To make a diagnosis, solid evidence (such as a history corroborated by friends and relatives) is needed that alcohol consumption is not excessive (eg, < 20g/day) and serologic tests should show no have hepatitis B and C (i.e. hepatitis B surface antigen and hepatitis C virus antibody should be negative).
Liver biopsy shows lesions similar to those in alcoholic hepatitis, often including large fat droplets (lenticular fatty infiltration) as well as pericardial fibrosis or "chicken wire". Indications for biopsy include unexplained signs of portal hypertension (eg, splenomegaly, cytoreduction) and unexplained elevations of aminotransferases lasting > 6 months in patients with diabetes diabetes, obesity or dyslipidemia.

Sinh thiết là phương pháp chẩn đoán gan nhiễm mỡ
4.3. Diagnostic imaging - Liver imaging tests, including:
Increased echoes on ultrasound; Decreased liver attenuation on CT; Increased fat signal on magnetic resonance imaging (MRI) may suggest NAFLD. Noninvasive measures of fibrosis such as transient elastography (test that uses both ultrasound and low-frequency elastography), ultrasound elastography, or MR elastography can be assessed. severity of steatosis as well as estimates of fibrosis, thus eliminating the need for liver biopsy in many cases. Transient elastography and ultrasonic elastography may be limited by body habits (too big/too fat for enough ultrasound waves to penetrate), while MR elastography is not. However, these tests cannot identify the typical inflammation of NASH and cannot distinguish NASH from other causes of fatty liver.
Outbound NIH Elastography is a newer type of imaging test that can help determine if you have advanced cirrhosis. In some cases, your doctor may order an elastography test to measure the stiffness of your liver. Increased stiffness of the liver can be a sign of fibrosis. The commonly used types of elastography are:
Vibration-controlled transient elastography, a special type of ultrasound; Absolute wave elastography, another type of ultrasound to detect increased stiffness of the liver; Elastic Magnetic Resonance, a special type of MRI that measures the stiffness of the liver. To diagnose NAFLD, signs of steatosis must be detected by imaging or biopsy, heavy alcohol consumption must be ruled out, and other causes of fatty liver disease must be ruled out.
A thorough history is important to rule out other potential causes of fatty liver disease such as alcohol, drug or drug use. Viral hepatitis may also have to be ruled out.
Usually, clinical imaging, blood tests, and imaging techniques will suffice to diagnose NAFLD. Most patients do not need a tissue sample by biopsy. However, biopsy is the only method that can distinguish NAFLD from NASH.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: niddk.nih.gov, stanfordhealthcare.org, msdmanuals.com